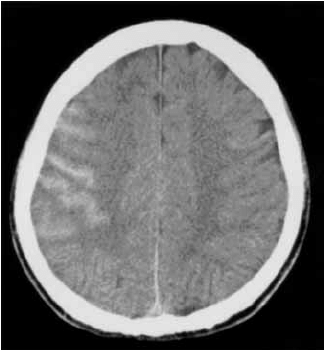
Neurosurgical involvement in the management of simple traumatic brain injury (TBI) has been slowly dwindling over the past several years. This is the result of the general consensus that very few of these patients progress to need neurosurgical procedures.
A group at Wright State University in Dayton sought to define the progression of one specific finding in TBI, the subarachnoid hemorrhage (SAH). Secondarily, the wanted to determine if a neurosurgery consultation was warranted in these patients.
They performed a five year retrospective review of their registry data, identifying patients with both mild TBI (GCS 13-15) and SAH. They excluded patients with any other brain lesion on CT.
Here are the factoids:
- 301 patients were enrolled during the 5 year period
- All had a neurosurgical consultation
- Time between the initial CT and a followup scan was about 11 hours
- 91% showed stable or resolving SAH on the followup scan
- 9% showed a worsening SAH or additional lesions on the repeat scan
Bottom line: The authors conclude that initial neurosurgical consultation is not needed, since only 9% of patients have worrisome findings on repeat CT. They do, however, recommend that the practice of repeat scanning be continued because of this same number.
Our trauma service looked at this issue a year ago, and determined that most of these lesions either do not progress, or never require any intervention if they do, with a few notable exceptions. For that reason, we abandoned both neurosurgical consultation and repeat CT scans for patients with non-aneurysmal SAH, a single parenchymal hemorrhage, or linear skull fractures. We continue to do both for patients with epidural and/or subdural hemorrhage. You can download a copy of this protocol here.
Questions and comments for the authors/presenters:
- Did you look at platelet count or INR in the study. Were patients excluded based on abnormal values?
- Did every patient get a repeat scan?
- Break down the lesions in the 9% of patients who had some sort of progression or new finding. Did you see any common themes (age, chronic alcohol use, etc.)?
- Did you encounter any patients with “non-central SAH”, that might indicate an aneurysm? How were they dealt with?
- How has or will your trauma service change its practice based on your findings.
Click here to go the the EAST 2017 page to see comments on other abstracts.
Related posts:
- Download the “no neurosurgery protocol” used at Regions Hospital
- Can TBI be managed without neurosurgeons?
- Can TBI be managed without neurosurgeons? Part 2
- When to worry about subarachnoid hemorrhage
Reference: Management of subarachnoid hemorrhage (SAH) by the trauma service: are repeat CT scanning & routine neurosurgical consultation necessary? Poster #16, EAST 2017.