Dry Seal Chest Tube Suction Systems
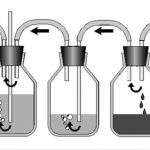
The original chest tube collection system traditionally consisted of three chambers. The picture above shows the classic three bottle system (which I actually remember using during residency). On the left is the suction control bottle that determines how much suction is applied to the patient. The middle bottle provides one way flow of air out of the patient, the so-called water seal bottle. Finally, the right bottle collects any fluid from the pleural space.
Collection systems used in hospitals are much more tidy than this, wrapping all three into one modular unit. However, if you look closely you can identify parts of the system that correspond to each of the bottles.
The problem with the older systems is that they typically require water in the “water-seal” chamber to maintain one-way flow out of the patient. If this chamber is compromised by knocking the system over (see this post), air may be able to enter the patient’s chest, giving them a big pneumothorax.
Management of chest tube collection systems by EMS is tough. It’s very easy to tip the system during air or ground ambulance runs, putting the patient at risk. Some manufacturers have developed so called “dry-seal” systems that use a mechanical one-way valve to avoid this problem.
I have not been able to use one of these systems yet. Here is my take on the pros and cons:
- Pro – immune to tip-over and malfunction of the water-seal chamber
- Con – more difficult to detect an air leak. Current models require either injection of a small quantity of water, tipping the system, or converting to a water-seal system.
- Con – no literature regarding safety of this relatively new technology
Bottom line: Looks like a great idea to me, especially for EMS use. Once they get to the hospital, the unit can be changed to a water-seal system or a larger dry-seal system with the water injection port inthe dry-seal chamber.