CT scan is a valuable tool for initial screening and diagnosis of trauma patients. However, more attention is being paid to radiation exposure and dosing. Besides selecting patients carefully and striving for ALARA radiation dosing (as low as reasonably achievable) by adjusting technique, what else can be done? Obviously, shielding parts of the body that do not need imaging is simple and effective. But what about simply changing body position?
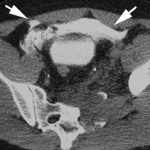
One simple item to consider is arm positioning in torso scanning. There are no consistent recommendations for use in trauma scanning. Patients with arm and shoulder injuries generally keep the affected upper extremity at their side. Radiologists prefer to have the arms up if possible to reduce scatter and provide clearer imaging.
A recently published article looked at arm positioning and its effect on radiation dose. A retrospective review of 690 patients used dose information computed by the CT software and displayed on the console. Radiation exposure was estimated using this data and was stratified by arm positioning. Even though there are some issues with study design, the results were impressive.
The dose results were as follows:
- Both arms up: 19.2 mSv (p<0.0000001)
- Left arm up: 22.5 mSv
- Right arm up: 23.5 mSv
- Arms down: 24.7 mSv
Bottom line: Do everything you can to reduce radiation exposure:
- Be selective with your imaging. Do you really need it?
- Work with your radiologists and physicists to use techniques that reduce dose yet retain image quality
- Shield everything that’s not being imaged.
- Think hard about getting CT scans in children
- Raise both arms up during torso scanning unless injuries preclude it.
Reference: Influence of arm positioning on radiation dose for whole body computed tomography in trauma patients. J Trauma 70(4):900-905, 2011.