The debate over incidental appendectomy has waxed and waned over the years. And for the most part, it has nearly permanently waned in general surgical cases for now. But every once in a while, I am asked about incidental appendectomy during trauma laparotomy. Is it a good idea? What reasons could there possibly be for doing it?

In the old days, we would frequently do an incidental appendectomy because… well, just because we were there. The surgeon was in the midst of a general surgical case, typically an open one, and this normal little appendix was staring us in the face. The justification was usually, “We’ll save him/her another operation in the future in case he develops acute appendicitis.”
Legitimate reason? It took many years for the literature to develop, but it finally did. Here are the reasons we figured out not to do it:
- Despite how innocuous a procedure seems, there is a measurable uptick in complication rates. This is true in the usual clean contaminated general surgery cases. Some papers also noted an increased mortality when the appendectomy was added to a cholecystectomy case. In a trauma procedure with bowel injury and contamination, it’s a bit harder to see the correlation. But any time we cut or staple something out, there is always the possibility that it might break down.
- Cost increases in laparoscopic cases if additional ports and equipment are needed for the appendectomy. This doesn’t apply to major trauma cases since we better not be doing them laparoscopically!
- The appendix is not the useless vestigial structure we initially thought. Evidence shows that it is a repository for the gut microbiome, which can help repopulate the colon with bacteria after a serious insult like prolonged antibiotic administration. Unnecessary removal may ultimately interfere with gut health and disease.
Can acute appendicitis develop after trauma laparotomy? Sure, at any time. Thankfully, it’s not very common. The presenting complaints are the same as we learned in the doctor books. However, the location of the pain and tenderness may not be in the classic location, depending on the post-trauma anatomy and presence of adhesions.
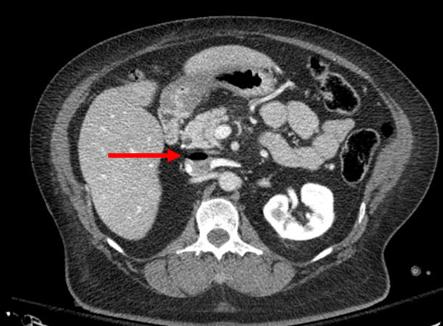
Bottom line: Incidental appendectomy is no longer indicated for just about anything, including trauma laparotomy. If one of your patients presents with abdominal pain at any time, both post-traumatic and other causes must be considered. CT has become the standard for appendicitis workup and is extremely helpful in sorting out causes in the post-op trauma patient. Use it, and if it is one of the rare cases where appendicitis is actually present, then proceed with the usual and appropriate operative on nonoperative management.
References:
- Incidental appendicectomy with laparotomy for trauma. Br J Surg 62(6):487-9, 1975
- Appendicitis following blunt abdominal trauma. Am J Emerg Med 35(9):1386.e5-1386, 2017.
- Systematic review of blunt abdominal trauma as a cause of acute appendicitis. Ann R Coll Surg Engl 92(6):477-82, 2010.