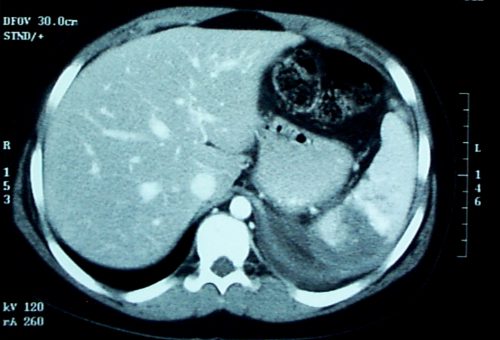
In my last post, I described the two types of solid organ “blushes.” I also described my thoughts on the natural history of these findings. Now, a multicenter study on the natural progression of the splenic “blush” has just been published. I found this paper very interesting, because it challenged some of my own existing beliefs. But once I read it, my enthusiasm faded.
The Western Trauma Association sponsored a multicenter (17 Level I and II centers) review of data collected prospectively over an unspecified period of time. Patients were excluded if their injury was older than 24 hours, if they had a previous splenic injury, and if they had any number of diseases or hereditary conditions that might affect the spleen. Strict definitions of nonbleeding and actively bleeding injuries were applied, and detailed information on intervention and outcomes was collected.

Here are the factoids:
- 200 patients were enrolled from 17 centers, but the paper does not state how long that took
- 20% were low grade (1 or 2) and 80 % high grade (3-5)
- 29% had a pseudoaneurysm, and 83% showed extravasation, which means that several patients had both
- 15% underwent early splenectomy, 59% underwent angiography, and 26% were observed
- For those with initial angiography, 6% had repeat angio and 7% eventually underwent splenectomy
- Of those were were initially observed, 9% had delayed angio and 8% underwent splenectomy
- Based on a read by an expert radiologist, an actively bleeding injury was associated with a 41% splenectomy rate
- The authors conclude that the majority of patients with spleen injury with pseudoaneurysm or extravasation are managed with angio and embolization and that splenectomy remains a rare event (??)
Bottom line: This paper just doesn’t do it for me. The biggest problem is that it is what I call a “we do it the way we do it” study. It examines how 17 different centers evaluate and treat patients with significant splenic injury. There was no guidance or guideline on how to treat, so they each did it their way. And the number of patients was small.
They don’t tell us anything about the use or effectiveness of angio by grade. Or whether the specific hospitals routinely rely on angio rather than just going to the OR for high grade injuries (typically if angio response times are long).
Unfortunately, this paper gives the appearance of containing a lot of interesting stuff. But a 15% initial splenectomy rate is not a “rare event” in my book. Everything published here is at odds with what I’ve observed over the years for centers with well developed management guidelines and easy access to angio (< 5% splenectomy rate in hemodynamically stable patients with nonoperative management).
My recommendation is to send all stable patients with pseudoaneursym and/or extravasation to angio immediately! Yes, some will have nothing found by the time they get to angio, and you’ll have to come up with a plan at that point. But most have something wrong, and it won’t stop until it’s been plugged up (or your patient bleeds to death, whichever comes first)!
This article has all the right buzzwords: multicenter, prospective data, etc. But it’s already been moved to my recycle bin.
Related post:
Reference: Natural history of splenic vascular abnormalities after blunt injury: A Western Trauma Association multicenter trial. J Trauma 83(6):999-1005, 2017.