How not to write your abstract! The full title is this:
Trauma Patients on New Oral Anticoagulation Agents Have Lower Mortality Than Warfarin
Now let’s look at what it really says. This was a retrospective trauma registry review from a single Level I trauma center. Over a 14 month period, 275 of 1994 admitted patients were on anticoagulants.
Here are the (misleading) factoids and my comments:
- Patients on warfarin had a higher mortality (13%) than those on new oral agents (NOA) (6%). (I can’t duplicate the statistical significance calculation)
- Patients taking any anticoagulant were admitted to an ICU more often (44-50% vs 36%). (Duh! This just shows their usual practice, nothing new)
- Patients on warfarin were more statistically likely to receive prothrombin complex concentrate. (Double duh! Because it doesn’t work for NOAs?)
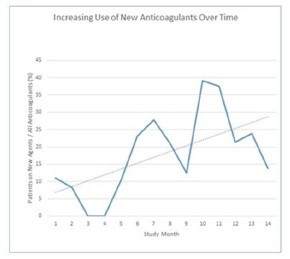
- The authors pointed out a trend toward more NOA use in this graph. (Really? It goes from 11 to 14 with wide monthly variations!)
Bottom line: This is why it’s so important to read the entire abstract and think about the stats. And ultimately, it’s even more important to read the whole paper! They don’t always say what you think they say!
Reference: Trauma patients on new oral anti-coagulation agents have lower mortality than those on warfarin. EAST 2016 Oral abstract #24.


