Foley catheters are a mainstay of medical care in patients who need control or measurement of urine output. Leave it to trauma surgeons to find warped, new ways to use them!
Use of these catheters to tamponade penetrating cardiac injuries has been recognized for decades (see picture, 2 holes = 2 catheters!). Less well appreciated is their use to stop bleeding from other penetrating wounds.
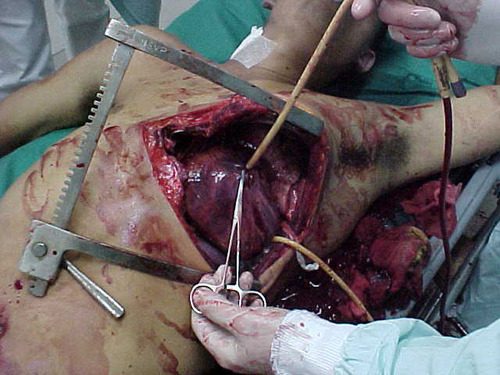
Foley catheters can be inserted into just about any small penetrating wound with bleeding that does not respond to direct pressure. (Remember, direct pressure is applied by one or two fingers only, with no flat dressings underneath to diffuse the pressure). Arterial bleeding, venous bleeding or both can be controlled with this technique.
In general, the largest catheter with the largest possible balloon should be selected. It is then inserted directly into the wound until the entire balloon is inside the body. Inflate the balloon using saline until firm resistance is encounted, and the bleeding hopefully stops. Important: be sure to clamp the end of the catheter so the bleeding doesn’t find the easy way out!
Use of catheter tamponade buys some time, but these patients need to be in the OR. In general, once other life threatening issues are dealt with in the resuscitation room, the patient should be moved directly to the operating room. In rare cases, an angiogram may be needed to help determine the type of repair. However, in the vast majority of cases, the surgeon will know exactly where the injury is and further study is not needed. The catheter is then prepped along with most of the patient so that the operative repair can be completed.
Tomorrow: an off-label use for this catheter in abdominal trauma!