It’s fat embolism week! I’ll cover this uncommon, yet very important clinical condition in my next four posts.
Fat embolism syndrome (FES) is one of those clinical problems that trauma professionals read about during their training, then rarely ever see. Although the clinical manifestations are frequently mild, they can progress rapidly and become life-threatening. Over the next five days, I’ll try to help you better understand this condition, and provide details on diagnosis and treatment.
Fat embolism syndrome (FES) is a constellation of findings that arise from a single, unified cause: the escape of fat globules into the circulation (fat embolism). The ultimate resting places of those globules determine the specific manifestations of FES seen in clinical practice. When it occurs, it typically becomes apparent 24 to 72 hours after injury.
Simple fat embolism occurs to some degree any time tissues containing fat are manipulated or injured. It has been demonstrated during plastic surgical injections for cosmetic purposes and lipid infusions. It is more frequently seen with orthopedic injuries, especially those involving the femurs and pelvis. And it makes sense that the more fractures that are present, the more likely fat embolism will occur. Embolism is also known to occur when performing orthopedic procedures, particularly those involving the marrow cavity (intramedullary nailing), but has also been reported in total knee and hip procedures.
Fat embolism syndrome has a generally reported incidence of 1 – 10%, although I believe that is on the high side. I see a case every 3 – 4 years in a predominantly blunt, fracture-laden practice. Fat embolism without symptoms occurs much more frequently. A study from 1995 using transesophageal echo found evidence of emboli in 90% of patients with long bone fractures.
But how do these fat globules get into the circulation and produce such chaos? We know that they can be mechanically pushed into small venules when tissues containing fat cells or bone marrow are injured. In bone, there are numerous small venules located throughout that are anchored to it. When the bone is fractured, these venules tear and are held open so yellow (fatty) marrow can be pushed into them.
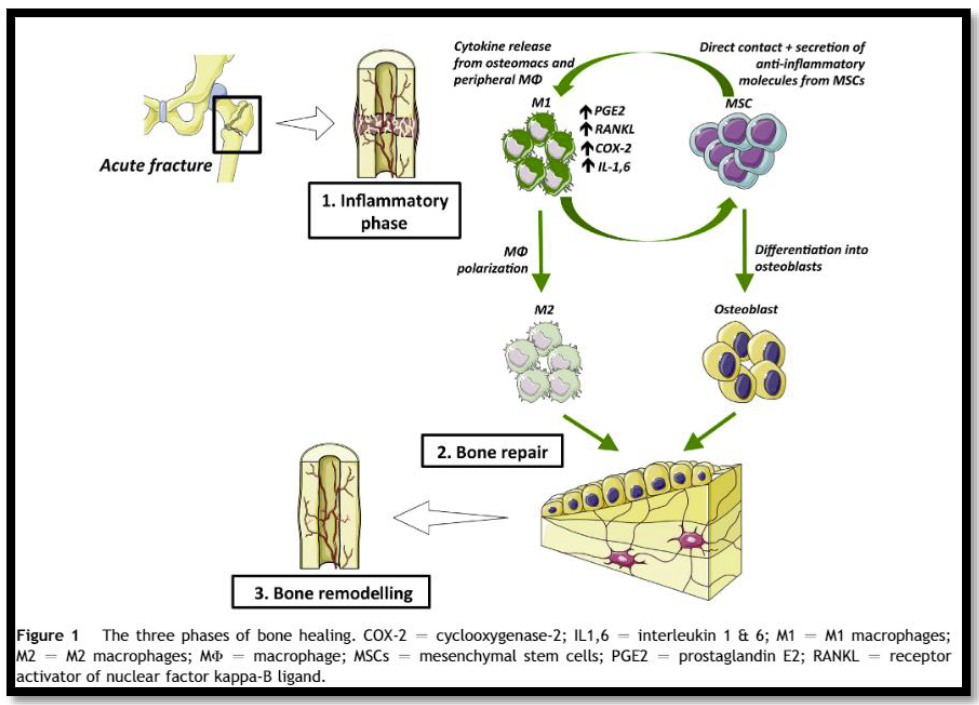
If enough emboli enter the blood stream, they may accumulate in the end vessels of tissues and block flow. Although this is a simple and appealing explanation, it may not be the full story. If the emboli primarily occur during and after injury, why does it take several days for the full-blown syndrome to develop?
A likely explanation is that the fat globules begin to degrade while in the circulatory system. Breakdown into free fatty acids results in the release of a cascade of cytokines and other mediators. The inflammatory response around the end vessels create the gross pathology that we associate with fat embolism syndrome.
In the next post, clinical manifestations of fat embolism syndrome.