Pelvic Trauma Radiographs Demystified
Although we are becoming increasingly reliant on CT scans for diagnosis, plain old radiographs still have their place. This is especially true in pelvic imaging after trauma.
The most common pelvic radiograph obtained is the supine A-P view taken during trauma resuscitation. This image gives a quick and dirty look at the entire pelvis, from iliac crest to ischial tuberosity. The main areas of interest are the pubic symphysis and the SI joints, so if some of the periphery is cut off a repeat is not necessary prior to CT scan. This image helps predict the need for blood and pelvic compression devices.
If fractures are present, the orthopedic surgeons will generally request additional views in addition to the CT scan. The scan gives excellent detail, but the axial image slices are still not as good as a plain old radiograph in many cases.
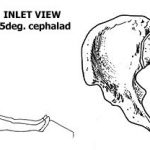
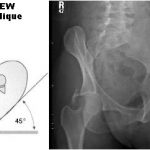
Inlet and outlet views are used to get a better look at the pelvic ring. The inlet view opens the ring up into a big circle (or oval) and allows identification of fractures of the sacrum or displacement of the SI joints, as well as changes in the pubic symphysis. The outlet view shows any vertical displacements through the sacrum or SI joints well, and gives a better appreciation of some pubic fractures.
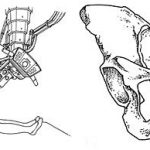
Judet views help demonstrate acetabular fractures by lining up the iliac wing with the xray tube. They can give additional information that the orthopedists use for determining operative or nonoperative management.
Rule of thumb: For major trauma patients, obtain an A-P pelvis radiograph if indicated by mechanism of injury or physical exam. Perform CT scan of the abdomen and pelvis if indicated. If a pelvic ring fracture is identified, obtain inlet and outlet radiographs before calling your orthopedic surgeon. If an acetabular fracture is seen, obtain Judet views before calling.