Temporal Bone Fracture
The temporal bone is a very complicated and important piece of bone located at the base of the skull. It houses a number of structures vital to hearing and balance, and is a conduit for several important nerves. Most fractures are due to blunt trauma, and although several classification systems exist, the majority are irregularly shaped and don’t lend themselves to easy categorization.
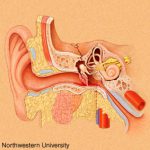
Clinically, a t-bone fracture should be suspected anytime that blood is seen in the ear canal or behind the eardrum after blunt head trauma. Patients may complain of dizziness or hearing loss. Examination may demonstrate some nystagmus in some cases. Most of the time, the diagnosis will not be made until a head CT is performed. The diagram above shows why this fracture can cause hearing problems (middle ear) or dizziness (inner ear).
There is usually no specific surgical intervention needed for this fracture. However, two important functional exams must be completed once diagnosed: facial nerve function and hearing. The facial nerve exam should document whether only portions of the nerve are affected vs all branches, and whether there is at least partial function. In head injured patients that can’t follow commands, even a grimace can demonstrate some function.
The ideal hearing test is carried out with a tuning fork. However, this is not usually convenient in acute trauma patients. Whispering and rubbing fingers near the patient’s ear can be used as a quick and dirty test. Awake patients will be able to tell you if their hearing is decreased.
Bottom line: Suspect temporal bone injuries in patients with any signs of basilar skull fracture. If the diagnosis is suspected or confirmed by CT scan, document the best facial nerve and hearing exam that you can. Contact your facial surgeon once the diagnosis is confirmed, and call them urgently if there is any loss of facial nerve function. Thin cut CT scans of the temporal bone are generally not necessary, and should not be ordered automatically unless the facial surgeon needs it for a specific reason.