I’ve written quite a bit about the challenges of diagnosing blunt carotid and vertebral artery injury (BCVI) in adults. And now some papers on the potential danger to pediatric patients are beginning to surface.
I think it’s time to repost and update my series on BCVI. I’ll start with the basics, like nomenclature. I’ll then move on to how often we actually encounter it. This will include new information on younger patients.
I’ll dig into the various screening systems, and will include new information from some recent pediatric papers. The, I’ll finish up with how to grade it and suggested treatment routines based on grade.
Lets start with the acronym itself. There seems to be some confusion as to what BCVI actually stands for. Some people believe that it means blunt cerebrovascular injury. This is not correct, because that term refers to injury to just about any vessel inside the skull.
The correct interpretation is blunt carotid and vertebral artery injury. This term refers to any portion and any combination of injury to those two pairs of vessels, from where they arise on the great vessels, all the way up into the base of the skull. Here’s a nice diagram:
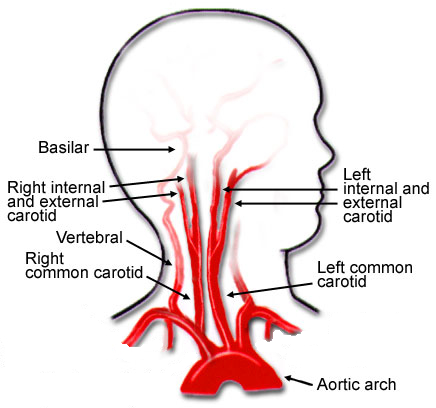
Note that we will be excluding the external carotid arteries from this discussion, since injuries to them do not have any impact on the brain. They can cause troublesome bleeding, though.
These arteries are relatively protected from harm during blunt trauma. But given enough energy, bad things can happen. Fortunately, injuries to these structures are not very common, but unfortunately many trauma professionals under-appreciate their frequency and severity.
In the next post, we’ll explore the incidence of this injury in both adults and children. Is it truly as uncommon as we think?