The rapid infusion pump is a mainstay of high volume trauma resuscitation. According to the manufacturers, these devices can now deliver fluids at up to 1000 ml/minute. Or can they?
Here is a chart from the manufacturer of the Belmont rapid infuser. This shows the (theoretical) flow rates achievable for each of their two devices (max flow rate of 750 ml/min and 1000 ml/min models). The charts show the maximum flow rates for crystalloid or blood for various sizes of IV catheters that are 2″ long.
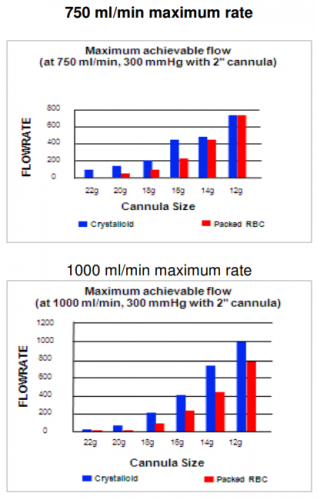
Notice two things:
- The flow rate decreases exponentially as the size of the IV catheter decreases
- The difference in flow rate between blood and crystalloid diminishes as the catheter size increases
These observations can be explained by something I’m sure you haven’t thought about since high school physics: Pouiseulle’s Equation. Of course you remember, right?
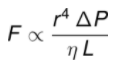
The equation states that the flow of a fluid (F) is proportional to the fourth power of the radius of the catheter and the pressure gradient across the two ends of it (delta P), and inversely proportional to the viscosity of the fluid (greek letter eta) and the length of the catheter (L).
What does this mean in practical terms?
- The pressure gradient is fixed at about 300 mm Hg (the pressure bag or pump) so you can essentially ignore this factor
- The viscosity (measured in centipoise) is based on the fluid begin given. Crystalloid (water) has a viscosity of 1. Whole blood has a viscosity of about 2.7, and packed cells are about 10. This means that our typical infusion of PRBC flows 10 times more slowly than saline.
- The length and diameter of the IV catheter are controlled by the trauma professional who inserts it, and it has a massive impact on flow. This is particularly true for the diameter (gauge), which varies directly as the fourth power.
So let’s put all these numbers together. Let’s assume that we are using balanced resuscitation and are infusing lots of blood, not crystalloid. The choice of IV catheter is the most important factor for a successful volume resuscitation! Here’s a table I constructed that lists the approximate relative flow rates for several catheter types. I use a 9 Fr introducer as the gold standard and have defined the flow rate for that device as 1.
| IV Catheter | Internal Radius | Length | Relative flow |
| 9 Fr Introducer | 1.5 mm | 10 cm | 1 |
| 14 Ga IV | 0.8 mm | 5 cm | 1/6 x |
| Triple lumen cath | 0.3 mm | 20 cm | 1/1265 x |
Bottom line: High-speed volume resuscitation forces us to squeeze a thick (and hopefully warm) liquid through a small straw into our patient’s vein. The smaller and longer the straw, the harder it is to do that. I think that people underestimate how much of an impact the choice of catheter makes.
Always use the largest and shortest possible access for rapid infusion. Ideally, this should be a large, straight introducer. Some have a side port (e.g. Cordis) at a right angle to the catheter, but this introduces some extra resistance and will slow the infusion rate. A large bore (14 Ga) short (2 inch) IV catheter is good, but will only flow at one sixth the rate of an introducer.
And never use anything with more than one lumen! The typical triple lumen catheter has three lines that are either 20 or 21 Ga. They are tiny and very long. Looking at the table above, you will be lucky to infuse a few cc’s per minute through one of these, compared to hundreds of cc’s via a straight introducer.
References:
- Internal diameter of IV catheters: Wikipedia
- Poiseuille’s law: cvphysiology.com/Hemodynamics/H003