In my last post, I reviewed a study that scrutinized reversal of direct oral anticoagulants (DOACs), and the outcomes of using various reversal agents. Today I’ll look at an abstract that compared in-hospital outcomes of elderly patients with severe TBI who were taking a variety of anticoagulant drugs, including DOACs.
The group at St. Joseph Mercy Hospital in Ann Arbor reviewed the dataset from the Michigan Trauma Quality Improvement Program database over a seven year period. To be included, patients needed to be at least 65 years old, suffer a fall, and have a significant head injury (AIS > 3). The final data consisted of records from 8312 patients treated at both Level I and II trauma centers across the state.
Here are the factoids:
- 40% of patients were taking antiplatelet agents, 13% warfarin, 4% DOAC, and the remaining half or so were taking nothing.
- The head injuries were severe, with mean AIS of 4.
- After adjusting for “patient factors”, mortality or hospital outcomes were 1.6x more likely when warfarin was used
- Complication risk increased 1.4x for warfarin and 1.3x for antiplatelet patients, but not for DOACs
- Hospital length of stay was a day longer in the warfarin group (6.7 days) vs about 5.7 in the others
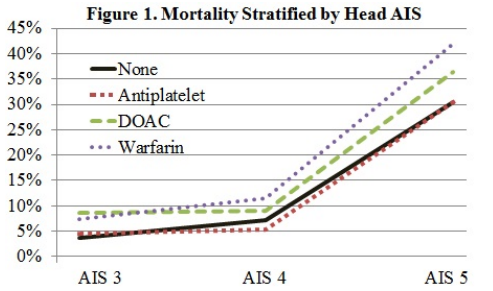
The authors concluded that elderly patients with severe TBI on DOACs fared better than those on warfarin. They stated that this could help alleviate concerns about DOACs in head trauma patients.
This is yet another interesting and surprising piece of the TBI on anticoagulants puzzle! It is obviously limited due to its retrospective database nature, which prevents us from asking even more interesting questions of this dataset. And it completely prevents us from looking at the specifics of each case including decision making, imaging, etc. But it’s a good start that should prompt us to find even better sources of data to tease out the details we must know in order to improve this patient group’s care.
Here are my questions for the presenter and authors:
- I am very interested in the “patient factors” that were adjusted for to try to normalize the groups. Please describe in detail the specific ones that were used so we can understand how this influenced your results.
- This information is intriguing, suggesting that warfarin is more evil that DOACs. What is the next step? What shall we do to further elucidate the problems, and how can we ameliorate the mortality and complication effects?
This is more good stuff about DOACs, and I can’t wait to hear the details.

