This post is a favorite, and I’m publishing it again since I just finished my “When To Call” series.
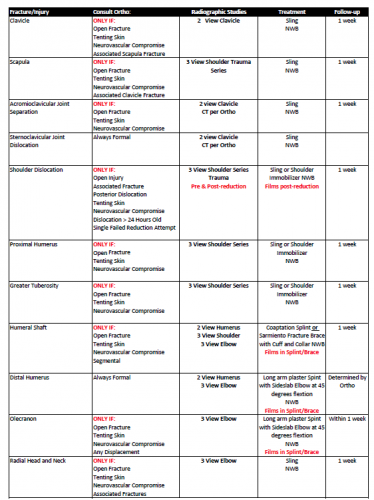
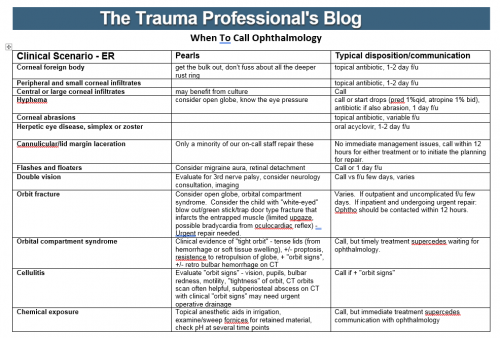
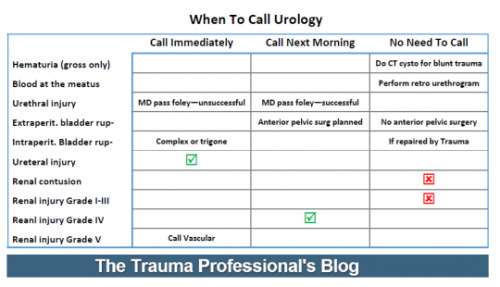
Trauma surgeons often rely on consultants to assist in the care of their patients. Orthopedic surgeons and neurosurgeons are some of the more frequent consultants, but a variety of other surgical and medical specialists may be needed. I have found that providing a set of guidelines to consultants helps to ensure quality care and provide good communication between caregivers and patients / families.
We have disseminated a set of guidelines to our colleagues, and I wanted to touch on some of the main points. You can download the full document using the link at the bottom of this post.
In order to deliver the highest quality and most cost-effective care, we request that services we consult do the following:
- Please introduce yourself to our patient and their family, and explain why you are seeing them.
- Although you may discuss your findings with the patient, please discuss all recommendations with a member of the trauma service first. This avoids patient confusion if the trauma team chooses not to implement any recommendations due to other patient factors you may not be aware of.
- Document your consultation results in writing (paper or EMR) in a timely manner.
- If additional tests, imaging or medications are recommended, discuss with the trauma service first. We will write the orders or clear you to do so if appropriate, and will discuss the plan with the patient.
- We round at specific times every day and welcome your attendance and input.
- Please communicate any post-discharge instructions to us or enter in the medical record so we can expedite the discharge process and ensure all followup visits are scheduled.
Bottom line: A uniform “code of behavior” is important! Ensuring good patient communication is paramount. They need to hear the same plans from all of their caregivers or else they will lose faith in us. One of the most important lessons I have learned over the years is that you do not need to implement every recommendation that a consultant makes. They may not be aware of the most current trauma literature, and they will not be familiar with how their recommendations may impact other injuries.
Click here to download the full copy of the Regions Hospital Trauma Services consultant guidelines.