More MTP stuff! Every trauma center has a massive transfusion protocol, and current literature encourages them to try to achieve an “optimal” transfusion ratio. The literature has converged on a red cell to plasma ratio of somewhere between 1:1 and 2:1. Less has been written about platelet ratios, and trauma centers often don’t pay as much attention to this ratio when reviewing MTPs.
But is it important? The trauma group at the Massachusetts General Hospital examined the impact of platelet ratios on mortality in patients undergoing MTP. This was another TQIP data analysis, performed over a nine year period.
The authors defined massive transfusion as ten or more units of PRBC in the first 24 hours, or any number of units of red cells, plasma, or platelets given within the first four hours. They also defined “balanced” as a ratio of RBC to FFP and RBC to platelets <2. Multivariate regression analysis was performed to gauge the impact of ratios and achievement of a balanced resuscitation on 24-hour mortality.
Here are the factoids:
- A total of 7,520 patients in the dataset underwent MTP
- Nearly 83% achieved RBC to FFP balance, but only 6% had RBC to platelet balance (!)
- Patients with both balanced FFP and platelets had the lowest mortality at 24 hours
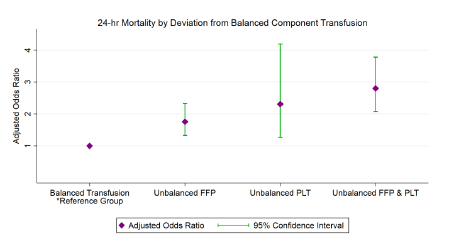
- Mortality increased by 2x with unbalanced plasma, a little more than 2x with unbalanced platelets, and 3x if both were out of balance (see figure)
The authors concluded that the platelet component of the MTP was frequently out of balance, and that it is associated with mortality to a greater degree than with unbalanced plasma.
Bottom line: This paper confirms my observations that trauma centers pay a lot more attention to the red cell to plasma ratio and don’t get as excited when the platelets are out of line. Part of this is probably due to confusion over how to count platelet packs. Typically they are delivered in packs called “pheresis” or “apheresis.” Each is the equivalent of about 6 units of platelets (check with your blood bank for more exact numbers). This means that a ratio of 6 RBC to 5 plasma to 1 platelets would be considered balanced. But a ratio of 28:28:2 would not.
According to this abstract, the use of sufficient platelets is important. This makes sense. However, the exact mechanism cannot be determined from this type of study. It could be a direct effect of not having enough platelets to form good clot. Or it could be something completely outside the clotting mechanism, just an association with something in the care processes that occurs as these patients undergo resuscitation.
The why doesn’t matter so much, though. This abstract presents compelling data that suggests that we really need to pay attention to the platelet ratios given during the MTP. They should be analyzed just as closely as plasma ratios during PI review, and changes to the MTP process implemented to normalize this important ratio.
Here are my questions for the authors and presenter:
- There is a statement in the methods section that is not clear. “only patients with steady RBC/PLT and RBC/FFP ratios between 4-and 24-hr were analyzed.” What is your definition of “steady?”
- Did you see any mortality patterns in the data you analyzed that might suggest why lower platelet volumes were more deadly?
This was a nicely done abstract, and I look forward to the live presentation and the finished manuscript!
Reference: DON’T FORGET THE PLATELETS: BALANCED TRANSFUSION AND THE INDEPENDENT IMPACT OF RBC/PLT RATIO ON MORTALITY IN MASSIVELY TRANSFUSED TRAUMA PATIENTS. EAST 25th ASA, Oral abstract #1.

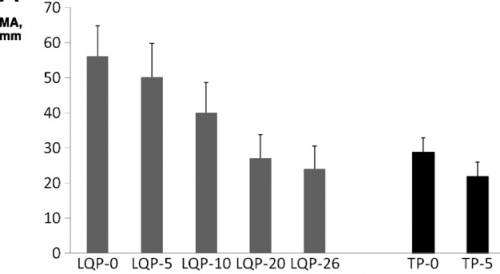 (TEG MA for liquid (LQP) and thawed (TP) plasma
(TEG MA for liquid (LQP) and thawed (TP) plasma