What The Heck? The Answer
Obviously, there’s a big knife in this image, and it appears to coincide with our patient. Remember, you can’t tell the relative positions of objects in the z axis in a two dimensional radiograph. However, you know that it is not on top of or under this patient, because there is an obvious hemothorax.
First, this patient should have been a trauma activation, since there is a penetrating injury of the chest. The first decision point is based on vital signs: is the patient hemodynamically normal? If not, do the essentials quickly (quick exam, lines, blood draw for blood bank) and move to the OR. The quick exam is important, especially of the back, since you may not see it for the next few hours and additional injuries there could be trouble.
If the patient is stable, then it’s time to do the essentials and figure out what you are going to need to do in the next hour. A chest xray can be very helpful. However, given the size of the knife and the fact that it appears to be buried to the hilt allows you to calculate the trajectory in your mind. The only question is if it went in far enough to enter the abdomen.
The xray shows a moderate hemothorax and a tip that extends well into some part of the abdomen, no matter how you look at it. It has also come alarmingly close to the heart. If the knife had not penetrated as deeply and was obviously only in the chest, then removal of the knife with insertion of a chest tube would be appropriate.
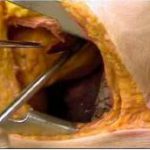
However, in the case of this xray, the patient still needs to go to the OR. The chest and abdomen need to be prepped and the abdomen opened first. Once the knife is located, the next steps can be planned. If there is concern for the heart, the pericardial surface of the diaphragm can be opened to look for blood. If found, extension of the laparotomy incision into a sternotomy is appropriate for cardiac repair. If not, the tip of the knife should be visualized and the weapon slowly removed under direct vision. Any bleeding structures can be dealt with first as it goes, followed by any injuries to a hollow viscus.