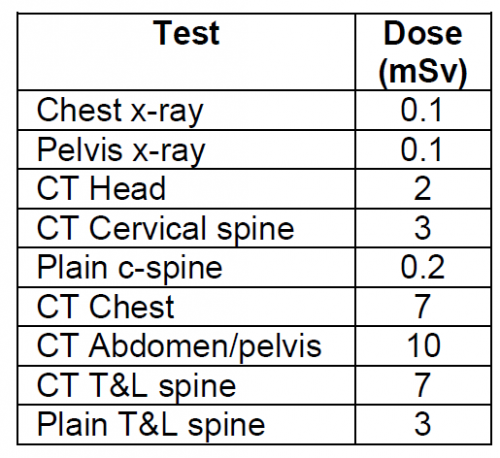
I periodically publish a chart that shows how much radiation exposure our patients get from various trauma imaging studies. For reference, here it is:
| Test |
Dose (mSv) |
Equivalent background
radiation |
| Chest x-ray |
0.1 |
10 days |
| Pelvis x-ray |
0.1 |
10 days |
| CT head |
2 |
8 months |
| CT cervical spine |
3 |
1 year |
| Plain c-spine |
0.2 |
3 weeks |
| CT chest |
7 |
2 years |
| CT abdomen/pelvis |
10 |
3 years |
| CT T&L spine |
7 |
2 years |
| Plain T&L spine |
3 |
1 year |
Millimeter wave
scanner (that hands
in the air TSA thing at
the airport) |
0.0001 |
15 minutes |
Scatter from a chest
x-ray in trauma bay
when standing one
meter from the
patient |
0.0002 |
45 minutes |
Scatter from a chest
x-ray in trauma bay
when standing three
meters from the
patient |
0.000022 |
6 minutes |
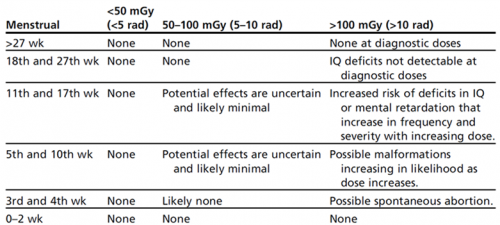
One of the issues that trauma professionals gnash our teeth about is how much radiation the baby gets when we perform these studies on pregnant women. Well, here is just what you need. Another chart! In order to avoid confusion, I will list effective doses to the fetus in milligrays (mGy), which is how much radiation is deposited in a substance. This is a little confusing, since doses are frequently listed in millisieverts which takes the specific organ and type of radiation into effect. In general, these two units are very similar for x-rays.
A useful rule of thumb is that if the fetal dose is less than 50 mGy during any trimester, the risk of an abortion or fetal malformation is about the same as from other risks to the pregnancy. The American College of Radiology notes that exposures less than 100 mGy are “probably too subtle to be clinically detectable.”
To help in your clinical decision making, I’ve added some extra information to the table regarding fetal exposure:
| Test |
Adult Dose (mSv) |
Fetal Dose (mGy) |
| Chest x-ray |
0.1 |
negligible |
| Pelvis x-ray |
0.1 |
negligible |
| CT head |
2 |
<1 |
| CT head and C-spine |
4 |
10 |
| CT chest |
7 |
<1 |
| CT abdomen/pelvis |
10 |
25 |
| Pan Scan (CTA chest, abdomen, and pelvis) |
up to 68 |
up to 56 |
| CT pulmonary angiogram |
up to 40 |
<1 |
Bottom line: We still have to think hard about how we image pregnant patients! There are some alternatives available to us, including the good old physical exam, conventional x-rays, and ultrasound. MRI is possible, but is a pain in the ass for many reasons.
CT of the head and cervical spine are fine for both mother and baby, and non-contrast imaging of the torso is within accepted limits of fetal exposure. However, the whole point of the torso scan in CT is to identify critical injuries that may lead to exsanguination like solid organ and aortic injuries. In general, those scans should always be ordered with contrast.
If clinical suspicion is high, it may be necessary to order these higher-dose studies anyway. If the mother has an unrecognized and potentially fatal injury, the baby will not survive either. There are many, many permutations of injuries and diagnostics. These cases will put your clinical judgment to the test, for sure!
References:
- Imaging Pregnant and Lactating patients. RadioGraphics 35:6, 1751-1765, 2015.
- Imaging of the pregnant trauma patient. RadioGraphics 34:3, 748-763,2014.
- Fetal doses from radio logical examinations. Br J Radiol;72(860): 773–780, 1999.