Is It Really Safe To Observe Occult Pneumothorax?
Occult pneumothorax is the most common incidental finding on CT imaging, occurring in 2% to 10% of trauma patients. By definition, an occult pneumothorax is a pneumothorax that is seen only on CT and not a conventional chest x-ray. When detected, the question that comes to mind is, will this patient need a chest tube?
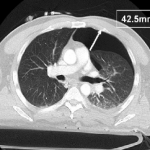
The AAST conducted a trial encompassing the experience at 16 Level I and II trauma centers around the US. They looked at injury severity, specific chest injuries, ventilator settings if on positive pressure ventilation (PPV) and size of pneumothorax. The size was calculated by measuring the largest air collection along a line perpendicular to the chest wall (see image above). Failure of observation meant that a thoracostomy tube was placed.
The 2 year study looked at a total of 448 occult pneumothoraces that were initially observed. Key findings of the study were:
- Injury severity was no different between failure and non-failure groups
- There was a 6% failure rate overall
- PPV alone was associated with an increased failure rate of 14%
- Surgical intervention requiring PPV was not associated with an increased failure rate
- Pneumothorax size > 7mm, positive pressure ventilation, progression of the pneumothorax, respiratory distress and presence of hemothorax were associated with failure.
- Pneumothorax size was not entirely reliable for predicting failure, since patients with sizes as small as 5mm on PPV and 3mm not on PPV failed in this series
Bottom line: Most blunt trauma patients with an occult pneumothorax can be safely observed. A followup chest x-ray should be obtained to look for progression. If the patient progresses, is placed on PPV, has a hemothorax or develops respiratory distress, have a low threshold for inserting a drainage tube. Maximum pneumothorax size may predict failure when large, but it can still happen with very small air collections.
Related posts:
Reference: Blunt traumatic occult pneumothorax: is observation safe? – results of a prospective, AAST multicenter study. J Trauma 70(5):1019-1025, 2011.
CT image courtesy of Journal of Trauma