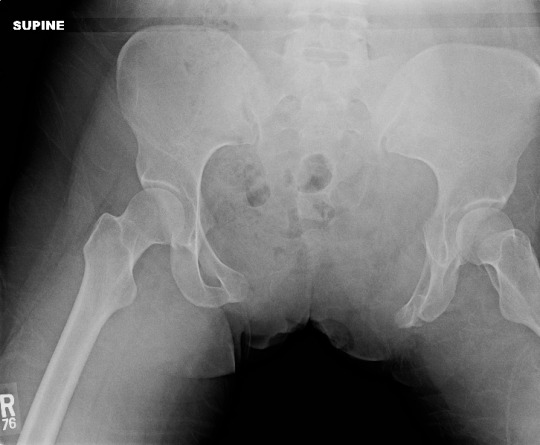
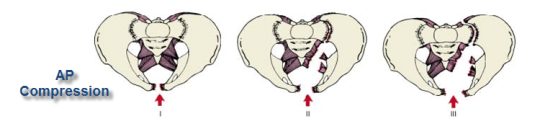
Yesterday, I wrote about the open book, A-P compression mechanism, pelvic fracture. In the “old” days, the recommended management for an unstable pelvis like these was application of an external fixator. In some textbooks, it was even suggested that this should be done (by orthopedics) in the resuscitation room. High volume trauma centers with ortho residents could actually pull this off, but not many others.
As the idea of pelvic orthotic binders caught on (T-POD, sheeting, etc) and was adopted by prehospital providers, and then trauma teams, the use of initial external fixation dropped off. But the idea that external fixation was the most desirable or most effective lingered on. A study from Memphis finally sheds some light on the answer to this question.

A 10 year retrospective review was carried out on patients presenting with multiple or severe pelvic ring fractures who had early stabilization of the pelvis. Stabilization consisted of external fixation early on, and gradually shifted to pelvic orthotic devices over the study period. They ultimately analyzed outcomes for 93 patients in each treatment group.
The authors found that transfusion needs were dramatically reduced with the orthotic devices (5 units vs 17 units at 24 hours) compared to the orthotics. About a quarter of patients in each group went to angiography, and even in those patients the transfusion need remained lower in the orthotic device group. Hospital length of stay was also significantly shorter in this group (17 vs 24 days). There was no difference in mortality.
Bottom line: Although this is a small, retrospective study it easily showed significant results and will probably never be repeated. Use of a pelvic orthotic device (POD) resulted in less blood replacement and shorter stays in hospital. This technique is simple, cheap and quick, an ideal combination. But does a sheet count as an orthotic device? We don’t know. It’s really cheap, but probably a bit less controlled than a POD. If you have a real POD in your ED or your ambulance, use it. If not, apply the sheet, which will be described tomorrow with other binders.
Tomorrow: what’s the “best” pelvic binder?
Reference: Emergent pelvic fixation in patients with exsanguinating pelvic fractures. JACS 204:935-942, 2007.