Nonsurgical admissions are a concern for most verified/designated trauma centers. Under the current 2014 Resources for Optimal Care of the Injured Patient, all trauma patient admissions to a nonsurgical service must be concurrently reviewed by the trauma program. This process guards against trauma patients sneaking into the hospital on medicine services where the quality of the care for their injuries may not be monitored.
Typically, this requirement is met by having the trauma program manager (TPM), trauma PI coordinator (TPIC), or registrar run a daily admission report and mark patients with a potential trauma diagnosis for further review. Some clinician then reviews the patient in person or via a chart check. No further attention is needed if the patient has low acuity injuries or has been seen by the trauma or other surgical service. If not, additional scrutiny is recommended to identify patients who might be better off with a trauma service consult or even a transfer of service.
The trauma group at the Charleston Area Medical Center in West Virginia postulated that adopting a trauma nurse practitioner (TNP) model to provide care for patients otherwise admitted to a hospitalist service would improve care and decrease nonsurgical admissions. The nurses were supervised directly by the trauma attending surgeons.
They analyzed retrospective registry data during a 22-month period and compared nonsurgical admission rates with the same data for the preceding three years. Several performance metrics were evaluated, including length of stay and those statistics hospitals love to watch, discharge orders placed by noon, discharge location, and time to operating room.
Here are the factoids:
- A total of 749 patients were admitted to the TNP service and 651 to hospitalist services
- Patients in the TNP group were significantly younger (59 vs. 76) and more likely to be male
- ISS was the same, but the TNP service patients had slightly more injuries (1.6 vs. 1.2) overall, and their patients were more likely to require an operation
- The number of comorbidities was higher on the hospitalist service (2 vs. 1.6)
- Hospital length of stay was one day shorter in the TNP group, which was significant
- TNP service patients were more likely to discharge home rather than to a skilled nursing facility
- Time to OR for the TNP patients was significantly shorter by 11 hours
- 30-day readmission rates were the same
- The percentage of patients admitted to a nonsurgical service decreased from 20% to 14% after implementation
The authors concluded that the nonsurgical admission rate declined significantly, and several performance metrics also improved. In addition, the decreased length of stay was projected to result in a decrease of over $876,000 in hospital charges throughout the study.
Bottom line: This study illustrates some potential differences that surface when patients are admitted and managed by a trauma service rather than a hospitalist service. I say potential because there are a lot of confounders here.
The patients on the two services were very different. Although the TNP service patients had slightly more injuries (1.6 vs. 1.2), their ISS was identical. They also had fewer comorbidities. There appears to be some selection process in play here, but it was not explicitly stated in the paper. It also appears that older and more complicated patients, in terms of their comorbidities, were admitted to the hospitalists. Those with injuries more likely to require surgery were admitted to the TNP service.
Nonsurgical admission rates definitely decreased, but without knowing the selection criteria, this could have been due to just the presence of the TNP service and the desire to admit patients to it. The decreased hospital LOS and higher discharge rate to home are impressive, but could this also be due to these patients’ younger age?
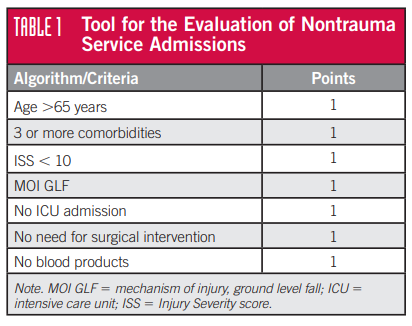
The final issue is that the rules have changed! Starting later this year with the implementation of the 2022 Resource Document, the 10% nonsurgical admission rate threshold will disappear. Now, all nonsurgical trauma admissions must undergo primary review via the PI process. If any issues are identified, the ISS is greater than 9, or there was no trauma or surgical consultation, they must be escalated to a timely secondary review by the trauma medical director. Gone are the days of retrospective reviews of these cases!
What to do? It’s a balancing act in terms of trauma service capacity and staffing. Ideally, most injured patients are best served on the trauma or surgical specialty service. Several papers have outlined improved outcome metrics with this arrangement. Utilizing TNPs or physician assistants to capture and manage appropriate patients can definitely be helpful.
An alternative is to integrate a hospitalist, preferably with geriatric expertise, into the trauma service so injured patients with more complex medical issues can be comfortably managed on the trauma service.
Reference: Rate of Nonsurgical Admissions at a Level 1 Trauma Center: Impact of a Trauma Nurse Practitioner Model. J Trauma Nurs 27(3):163-169, 2020.