In my last post on chest tube insertion technique, I reviewed a paper that compared chest tube insertion complications using two different trocar tips, blunt plastic and sharp metal. The sharp tip tubes caused more complications, although the study was weakened by the fact that the physicians inserting the tubes were complete newbies.
Today, I’ll discuss what the authors call a “best evidence topic” that reviewed the safety of the trocar technique. It is similar to a meta-analysis of available literature that attempts to reach a conclusion regarding this type of tube insertion. A literature search from 1946 to 2013 was conducted seeking to pull all papers on trocar chest tube insertion techniqes. A total of 258 papers were identified, but on closer inspection only 7 were identified that “provided the best evidence to answer the question.”
Here are the factoids from some of these papers:
- Tube malposition occurred significantly more often in a series of 106 trocar tubes inserted into 75 ICU patients
- In trocar tubes inserted for trauma, CT showed malplacement in 29% vs 19% with non-trocar tubes [This latter number seems very high to me!]
- A retrospective study of 1249 patients resulted in the trocar technique being abandoned due to severe lung and stomach injuries
- Use of trocar technique was associated with a significantly higher incidence of re-expansion pulmonary edema in 92 patients with spontaneous pneumothorax
- A poorly controlled prospective study showed 23 complications with trocar technique and none with blunt dissection. The denominator could not be determined.
Bottom line: Overall, the literature is just not good enough to answer this question. But it does provide some suggestions.
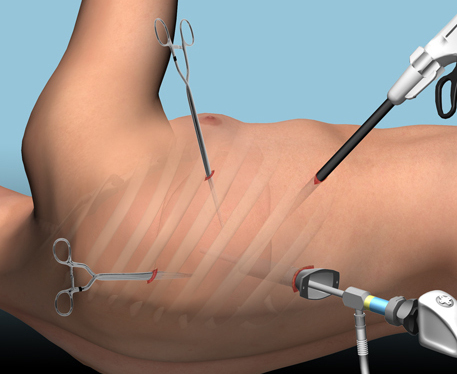
- Trocar insertion can be done well in experienced hands. Cardiac surgeons use these all the time, although sometimes they have the benefit of already being in the chest so they can visualize the point of entry and control the tip.
- Any chest tube insertion can go awry. It’s very important to learn proper technique, and take care to apply it faithfully, even in emergency situations.
- If you really like trocars and want to improve insertion safety, start with the blunt dissection technique first, sweep a finger inside the chest to ensure there are no adhesions, then insert the trocar tube to guide it into position. Please note that I do not believe that we can control the tube once the instrument (trocar or clamp) are removed from the chest. And the tube will work fine just about anywhere it ends up (unless that’s the spleen).
- Newbies should be supervised carefully and learn blunt insertion technique first. Be mindful that it is still possible to pass the insertion clamp into the same structures as a trocar if you are not careful. My practice is to place my fingers about 2 cm from the tip of the clamp as I push it through the pleura. If the pleura gives way more easily than anticipated, by fingers will keep the clamp from going too far into the chest.
- Always mark your insertion spot before prepping. This will generally be lateral to the nipple in men, so always prep the nipple into your field as a landmark.
- Always be careful!
Reference: Is the trocar technique for tube thoracostomy safe in the current era? Interactive CV and thoracic surg 19:125-128, 2014.