Medicine is full of conditions with eponyms. Trauma is no exception. There’s the Mattox maneuver and the Cushing response, to name two. Many times, the name is just a kind of vanity plate for the discoverer of the condition. But in the case of the LisFranc injury (or fracture), it makes some sense. This injury is tough to describe in a sentence or two, let alone a few words.
Jacques LisFranc de St. Martin was a French surgeon and gynecologist (!) who described this condition in about 1815. It entails the fracture of the heads of the metatarsal bones and possible dislocation from the tarsals (the cuboid, navicular, and three cuneiform bones). This area is known as the LisFranc joint complex.
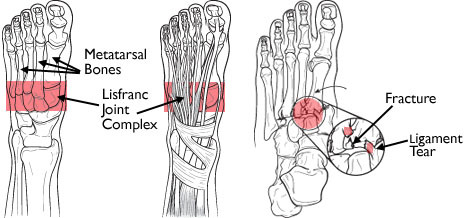
The injury can involve any or all of the metatarsals. The typical mechanism applies high energy across the midfoot, which can often be seen in head-on motor vehicle crashes. Crush injury to the proximal foot can also do this, such as running the foot over with a car. Occasionally, this injury pattern is produced with lower energy during sports play. In this case, the top of the foot is typically contacting the ground, plantar flexing it. At the same time, another player steps on the heel, grinding the foot into the ground (ouch). Interestingly, LisFranc did not describe the injury pattern or mechanism. His name is associated with the joint complex, and it is an injury to his joint complex.

Most of the time, the injury is obvious. There is usually notable pain and swelling of the foot. X-ray findings are generally not subtle. However, lower energy mechanisms may not cause much displacement, and initial imaging may not show the injury. If your patient starts to complain of pain in the midfoot when they begin to ambulate, think of LisFranc.
Treatment depends on the degree of displacement and the amount of disruption of the tarso-metatarsal joints. If minimal, a trial of nonoperative, non-weight bearing may be sufficient. But frequently, surgical reconstruction is required.