In my last post, I described a case where a fresh trauma patient was found to have an incidental finding of small, distal pulmonary embolus (PE) on her initial trauma evaluation. What should you do when you see this? Reflexively anticoagulate for months?
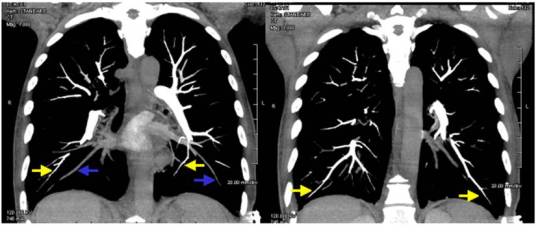
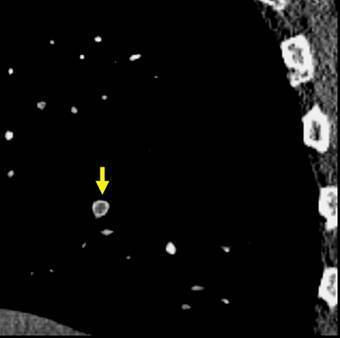
There are only a few papers dealing with this topic. One is from the MGH, which looked at their experience in screening for deep venous thrombosis (DVT) with duplex ultrasound and diagnosing PE with chest CT. They found that quite a few PEs were found that had no associated DVT in the legs or with clot in the pelvic veins. They also noted an interesting distribution: PEs with no DVT tended to be more distally located, and vice versa for those with DVT. This suggested that some PEs may not be emboli at all, but clot that forms spontaneously in the distal lung circulation.
Scripps Hospital in San Diego did some similar work. Only 31 of some 12,000 patients developed PE, and 19 of these had no identifiable DVT as a source. They also noted that these “de novo” PEs tended to be single and peripherally located. PE associated with DVT tended to be multiple and more central. They also noted an association with chest trauma (pulmonary contusion, rib fractures), blood transfusion, and pneumonia.
Bottom line: As usual, the literature is of little help in this relatively recently identified phenomenon. So what’s the trauma professional to do? Here’s my take. If a PE is found incidentally on the initial trauma evaluation, take a good history to see if there are any family members with clotting problems. Failing that, search for DVT using duplex ultrasound. If the PE is central or multiple, or there is a positive history or duplex screen, anticoagulate as you would any other patient with this problem. If not, carry out the usual prophylaxis and screening as laid out in your usual protocol (you have one, don’t you?), but don’t consider it a “real” PE. At least until we know more about this phenomenon.
Related posts: