Category Archives: General
Can TBI Be Managed Without Neurosurgical Consultation?
The standard of care in most high level trauma centers is to involve neurosurgeons in the care of patients with significant traumatic brain injury (TBI). However, not all hospitals that take care of trauma patients have immediate availability of this resource. An interesting paper looked at management of these patients by acute care surgeons.
The authors retrospectively reviewed all their patients who had a TBI and positive head CT managed with or without neurosurgery consultation over a two year period. They matched the patients with and without neurosurgical consultation for age, GCS, AIS-Head and presence of skull fracture and intracranial hemorrhage (parenchymal, epidural, subdural, subarachnoid). Neurosurgeons were available to the no-consult group if things went awry.
A total of 180 patients with and 90 patients without neurosurgical involvement were reviewed. Here are the interesting findings:
- Hospital admission rate was identical for both groups (88%)
- ICU admission was significantly higher if neurosurgeons were involved (20% vs 44%)
- Repeat head CT was ordered more than 3 times as often by neurosurgeons (20% vs 86%)
- Post-discharge head CT was ordered more often by neurosurgeons, but was not significantly higher (5% vs 12%)
- There were no neurosurgical interventions, in-hospital mortalities, or readmissions within 30 days in either group
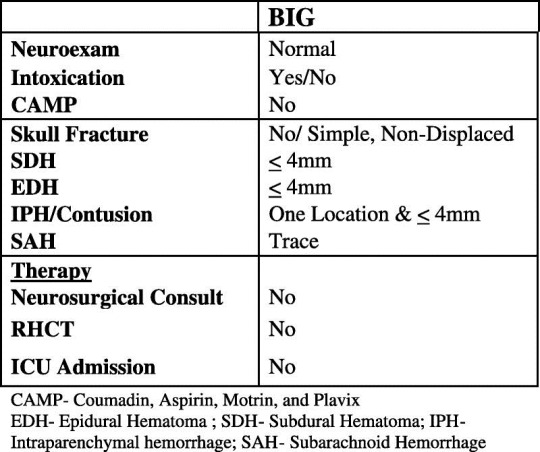
Based on this experience, the hospital adopted a set of guidelines for helping determine if neurosurgery should be consulted.
Bottom line: This work raises an interesting question: can general surgeons safely manage select patients with intracranial injury? The answer is probably yes. The majority of patients with mild to moderate TBI with small intracranial bleeds do well despite everything we throw at them. And it appears that surgeons use fewer resources managing them than neurosurgeons do. The keys to being able to use this type of system are to identify at-risk patients who really do need a neurosurgeon early, and having a quick way to get the neurosurgeon involved (by consultation or hospital transfer). Looking at the brain injury guidelines above, I am a little nervous about managing an epidural or contusion without one additional head CT. But this is certainly food for thought. As neurosurgery involvement in acute trauma declines, this concept will become more and more pertinent.
Related posts:
Reference: The acute care surgery model: managing traumatic brain injury without an inpatient neurosurgical consultation. J Trauma 75(1):102-105, 2013.
June Newsletter Released To Subscribers Friday!
The June Trauma MedEd Newsletter will be released to subscribers this weekend. I’ll be covering a topic no one wants to think about but everyone wants to know more about: Malpractice and trauma professionals. Articles include:
- What gets a physician sued?
- Trauma surgery malpractice risk
- Malpractice risk by specialty
- Nursing malpractice
- And more…
Anyone on the subscriber list as of 8PM Friday (CST) will receive it later over the weekend. I’ll release it to everyone else the middle of next week via the blog. So sign up for early delivery now by clicking here!
“Pull The Tube Back 2 Centimeters”
How often do trauma professionals hear that? Patients intubated in the ED (or before) almost universally have a chest x-ray taken to check endotracheal tube position. And due to variations in body habitus (and sometimes number of teeth), the tube may not end up just where we want it. So look at how deep or shallow it is and adjust it by the number of centimeters out of the correct position it should be, right?
Not so fast! A small, prospective study from Yale looked at endotracheal tube adjustment in ICU patients using tube markings and the patients incisors. Their “ideal” tube position has the tip between 2 and 4 cm from the carina. Any patients with an ET tube outside these parameters was included in the study. Here are the interesting tidbits:
- There were only 55 patients who met criteria for the study. No denominator information was give, so we can’t tell how good or bad the intubators were initially.
- Most tubes that needed adjustment were too far out. The median starting position was at 7cm above the carina (!),
- A smaller number were too deep (median position 0.7cm). These were mostly in women.
- The usual intended adjustment was 2cm. The actual distance moved after manipulation was half that (1.1cm).
Bottom line: Endotracheal tube repositioning based on tube markings at the incisors is not as accurate as you may think. Patient body habitus and reluctance to pull a tube out too far probably are factors here. So be prepared to readjust a second time unless you intentionally add an extra centimeter to your intended tube movement.
Related post:
Reference: Repositioning endotracheal tubes in the intensive care unit: Depth changes poorly correlate with postrepositioning radiographic location. J Trauma 75(1):146-149, 2013.
Why We’re Still Losing The Motorcycle Helmet Battle
Fewer and fewer states have good helmet laws any more. Part of the problem is political. But the other part, may be… the end user. Here’s a piece written by a doctor and published in the St. Paul Pioneer Press in 1994 about a case he saw in medical school:
“I was working in a rural emergency room one day when the ambulance brought in a 17-year-old who had been in a motorcycle accident. It had just started raining, and the road was slick; he’d tried to take a corner too fast and had laid the bike down and skidded quite a long way.
“Fortunately, all he had were crapes and bruises. he had no head injury.
“Just as I was finishing up with him, a policeman came in and brought the young man his helmet, which they had taken off him at the scene. it was obviously a fancy and expensive helmet. It was a full-face unit – shiny, multicolored, metal-flake.
“One entire side of the helmet was ruined. It was deeply gouged and had obviously scraped along the asphalt with considerable impact for quite a distance. In some places, it appeared that the entire thickness of the hard shell had been penetrated, and you could see the soft inner lining.
“The young man was obviously very lucky.
“He looked at the helmet, groaned and said: ‘Oh, man! I just bought that a week ago! What a waste of $150!’”


