Only you can prevent stupid
Category Archives: General
Is It Really Safe To Observe Occult Pneumothorax?
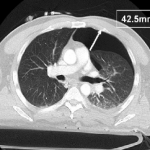
Occult pneumothorax is the most common incidental finding on CT imaging, occurring in 2% to 10% of trauma patients. By definition, an occult pneumothorax is a pneumothorax that is seen only on CT and not a conventional chest x-ray. When detected, the question that comes to mind is, will this patient need a chest tube?
The AAST conducted a trial encompassing the experience at 16 Level I and II trauma centers around the US. They looked at injury severity, specific chest injuries, ventilator settings if on positive pressure ventilation (PPV) and size of pneumothorax. The size was calculated by measuring the largest air collection along a line perpendicular to the chest wall (see image above). Failure of observation meant that a thoracostomy tube was placed.
The 2 year study looked at a total of 448 occult pneumothoraces that were initially observed. Key findings of the study were:
- Injury severity was no different between failure and non-failure groups
- There was a 6% failure rate overall
- PPV alone was associated with an increased failure rate of 14%
- Surgical intervention requiring PPV was not associated with an increased failure rate
- Pneumothorax size > 7mm, positive pressure ventilation, progression of the pneumothorax, respiratory distress and presence of hemothorax were associated with failure.
- Pneumothorax size was not entirely reliable for predicting failure, since patients with sizes as small as 5mm on PPV and 3mm not on PPV failed in this series
Bottom line: Most blunt trauma patients with an occult pneumothorax can be safely observed. A followup chest x-ray should be obtained to look for progression. If the patient progresses, is placed on PPV, has a hemothorax or develops respiratory distress, have a low threshold for inserting a drainage tube. Maximum pneumothorax size may predict failure when large, but it can still happen with very small air collections.
Related posts:
Reference: Blunt traumatic occult pneumothorax: is observation safe? – results of a prospective, AAST multicenter study. J Trauma 70(5):1019-1025, 2011.
CT image courtesy of Journal of Trauma
Trauma PI: When Is A Peer Issue Really A System Issue? (Part IV)
Yesterday I discussed loop closure for system issues. Today I’ll look at the interesting relationship between peer and system issues.
Although most PI issues that arise seem to be related to something done (or not done) by an individual, that doesn’t mean that the issue is peer-related. Frequently a significant portion of the problem is caused by a system issue. How can this be?
Let’s take the example of DPL. A physician performs a DPL in the trauma bay and the trauma PI program notes that it was performed without the requisite placement of an NG tube and urinary catheter first. At first look, this is a peer-related problem, right? Just counsel the doctor and everything will be better.
Wrong! Your PI program needs to assume that every apparent peer-related problem is a manifestation of one or more system issues. In my example, another DPL is performed 6 months later by a different physician, and once again the catheters are not inserted first. What gives?
I recently wrote that DPL was a dying art. Most institutions perform this procedure only a few times a year. People get rusty with uncommon procedures because they can’t practice. So instead of considering this a physician problem, look at it as a system problem. How can you keep them from forgetting something they seldom do? Simple! Attach a gastric tube and a urinary catheter directly to the DPL kit. When the physician grabs the kit, they will be instantly reminded of the need to insert them first. Problem solved.
Bottom line: always assume that people are doing their best to provide excellent care to their patients. Look closely for possible system problems that are keeping them from doing just that. Then put your thinking cap on and come up with some creative solutions.
Related posts:
Trauma PI: System Issue Loop Closure (Part III)
Yesterday I discussed loop closure for peer-related issues. Today I’ll delve into loop closure for system issues.
System issues are those that tend to involve multiple patients. They are not as easy to identify, because it may take a while for you to see a problem pattern emerging. And they are definitely harder to fix because they require a multi-faceted problem solving approach.
Here’s an example: You are presenting a complication (pulmonary embolism) in your trauma morbidity and mortality (M&M) conference. One of your colleagues notes that this is the third such presentation this year, which seems to be higher than previously. And come to think of it, the number of deep venous thrombosis presentations seems to be higher as well.
You ask your trauma registrar to run some reports on these complications, and you find that the incidence of both in your trauma patients has increased 80% over the previous year! Time to put on your thinking cap, review the literature and critically look at your care and what other centers are doing. You conclude that your trauma patient population hasn’t changed, but that your DVT surveillance and prophylaxis are spotty and vary considerably by physician.
Your solution consists of a new protocol or practice guideline that 1) identifies the risk level for each trauma patient, 2) defines what prophylactic measures will be used based on the risk assessment, and 3) determines what kind of screening will be done and how often. This protocol is implemented by your trauma operations committee, with all trauma physicians instructed to use it. It is monitored by your trauma program staff, and regular scorecards are sent to each physician. Regular reports detailing physician compliance and patient complications are made at each M&M or Trauma PI Committee meeting as well.
Six months later, registry data is reviewed again and you find that the incidence of DVT has decreased (but not to baseline because you are screening better and finding more), and the number of pulmonary emboli has dropped nearly to zero. Problem solved? Maybe. Periodic monitoring and continuation of the scorecard system is probably needed to make sure that the protocols are maintained.
What do you need to close the loop? You need a “folder” to save your information as I discussed previously. Since this problem involves many patients, it doesn’t fit as well into current registry packages that are oriented to single patient records. Whether your folder is paper or electronic, here are the items that need to be saved:
- Minutes from the first M&M meeting where the discussion reflects the recognition of the problem
- The registry reports that show the increasing incidence of the problem
- The new protocol and scorecard that were developed, along with any tracking tools
- The operations committee minutes showing approval of the protocol
- Completed scorecards for the physicians
- M&M minutes for meetings at which DVT/PE reports were given
- Registry reports that show the decreased incidence of DVT/PE. You can consider the item closed at this point.
- Any followup registry reports for monitoring done on a regular basis can be added to the folder later
As you can see, this is much more complicated than a peer issue. However, system issues show the value and strength of your trauma PI program. Trauma reviewers focus on how well you identify and address system problems because it is an indication of the maturity and power of your trauma program.
Related posts:
Trauma PI: Peer-related Loop Closure (Part II)
Yesterday I wrote about loop closure in general and what it is. Today I’ll cover the specifics of peer-related performance improvement issues and how loop closure works with them.
A peer-related issue typically involves a single trauma professional. In most cases, this is a physician, but may be a nurse, PA or other provider as well. These issues are most often related to care delivered to a single patient.
The trauma program can identify a peer-related issue in a number of ways, including (with examples):
- PI filter – delay to laparotomy by a surgeon
- Complication – intestinal anastomosis breakdown
- Resuscitation video review – nonsterile insertion of urinary catheter by a nurse or tech
- Word of mouth – “Geez, it took forever to get blood from the blood bank!”
- and many more!
Once identified, a “paper trail” must be started that documents the specific issue and the details of how it was found. This can be on a paper PI form, or an entry in your PI or trauma registry software package. The key is that you need to be able to track the progress as long as the issue is “open.”
Next, a determination is needed as to how the particular issue needs to be resolved. For physician items, that may occur via a group meeting (e.g. M&M conference) or a one on one meeting with an appropriate department leader (e.g. trauma medical director). For nursing items, each hospital typically has its own procedure (e.g. meeting with nurse manager).
Once the specific provider has been “re-educated”, final documentation of the process must be prepared. This may include a portion of the M&M meeting minutes or a letter or email message detailing the specifics of the discussion or retraining. All of the documentation collected, from opening of the PI issue to closure, must be preserved in a “folder” associated with this patient (remember, paper or electronic). Furthermore, an entry should be made in the credentialing file for the provider so that these items can be discussed in their annual review.
Here’s a specific example: a surgeon admits a patient with a CT-proven Grade IV splenic laceration. Although hemodynamically stable at first, they have frequent drops in blood pressure in the ICU that respond to crystalloid and several units of blood. After 6 hours of pressures dipping into the 70s and 3 units of blood, the blood pressure finally drops to 50 and won’t come back up. The surgeon takes the patient to the OR and performs a splenectomy. The patient recoveries, but remains on the ventilator for 5 days because of the large volume resuscitation that was given.
The delay to laparotomy PI filters are triggered, and the TPM and TMD place the issue on the Trauma M&M conference agenda. After discussion with all the faculty, the determination is that the patient should have gone to the OR after the first pressure drop in the OR. It is believed that the number of ventilator days would have decreased significantly as well. The delay is deemed a preventable complication. The TMD dictates the meeting minutes, detailing the specifics of the discussion, and noting that the involved surgeon was present.
The final folder for the patient will contain documentation of the filter violation, a copy of the minutes from the M&M conference, and a copy of the short memo dictated by the trauma medical director that was placed in the surgeon’s trauma credentialing file.
Related posts:
- Loop closure (Part I)
- Peer-related loop closure (Part II)
- System issue loop closure (Part III)
- Peer issue vs system issue (Part IV)
Please send questions you may have so I can discuss on Thursday and Friday!