Blood Transfusion With Component Therapy
About 40 years ago, blood banks started moving away from keeping whole blood and began separating it into components (packed cells, platelets, plasma, etc.) for more targeted use. For most uses, this is just fine. But what about trauma?
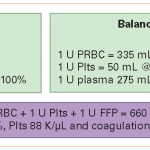
Trauma patients bleed whole blood. Doesn’t it make sense to give whole blood back? Much of our experience with massive transfusion is derived from our colleagues in the military. Two decades ago, the norm was to give 4 units of packed red cells or so, then give two units of plasma, and every once in a while slip in a bag of platelets. Our military experience seems to indicate that this 4:2:1 ratio is not optimal, and that something like 1:1:1 is better.
If you think about it, whole blood is already 1:1:1. Splitting it into components and then giving them back seems to be a lot of extra work (and expense) to accomplish the same thing as just giving a unit of whole blood. Plus it triples the exposure to infectious agents and antigens, since the components will usually come from three separate donors. Note that the data in the table above is true for fresh whole blood (not practical in civilian life); banked whole blood will lose some coagulation activity.
Is it time to think about supplying whole blood to trauma centers? And actually looking at whether the outcomes are better or not?