Airway management is one of the most anxiety provoking procedures performed by trauma professionals. The main fear is that the airway will be lost during attempts to secure it and patient demise will soon follow. Add some facial fractures, bleeding, and an “unfavorable body habitus”, and the average prehospital or ED provider is really on edge.
The next most common fear is that providing a definitive airway in a patient with a known (or even suspected) cervical spine injury could cause a catastrophic neurologic injury. This was first addressed back in 1989 (before the time of video laryngoscopy, and when flexible scopes were rarely available in the ED). The authors found no verifiable reports of such an injury in the entire English literature.
Over the years, a few case reports have cropped up. As in so much of the medical literature, causality is hard to prove. The patient was normal before anesthesia, and afterwards they were not. Had to be the intubation, right?
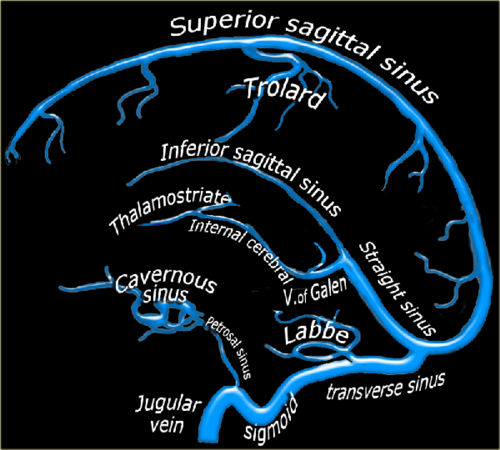
Not so fast! Let’s break it down and look at what we do know. Biomechanical studies have shown that the manipulation that occurs in direct laryngoscopy isn’t as bad as it looks. Studies in uninjured models are enlightening (minimal movement with blade insertion, slight rotational movements with blade elevation, and a little more rotation during the intubation). Most of this (slight) movement occurs from occiput to C2, with little motion at all at C3 and below.
But that was on an uninjured model. What about ones that simulate an injured spine? Specifically an injury in the upper spine area that we know moves?
- Cricoid pressure caused no appreciable changes in the spine
- Chin lift and jaw thrust reduced space available for the cord (SAC) by 1 and 2.5mm, respectively, and caused an angulation of about 4-5 degrees
- SAC narrowed by only 1.5mm, even with maximum flexion and extension
- Oral and nasal intubation narrowed SAC by 1.6mm, and resulted in a maximum of 2.5 degrees of rotation
- Video laryngoscopy results in about half of the rotational movement of direct laryngoscopy
References:
- Spinal cord injury and direct laryngoscopy – the legend lives on. Br J Anesth 84(6):705-709.
- Airway management in adults after cervical spine trauma. Anesthesiology 104(6):1293-1318, 2006.