Here’s an interesting trauma case, which comes from days of DPL. Although we don’t use this valuable technique very often, this one teaches an interesting lesson.
A middle aged female was involved in a high speed car crash. She was brought to the resuscitation bay as a trauma activation because the medics reported she had bilateral femur fractures, and her systolic pressures were in the 90’s.
As you proceed through the ATLS protocol, you call for blood to supplement your resuscitation fluids, and you also find that her abdomen is tender, with some right upper quadrant guarding. The femurs are placed in traction splints. FAST is generally negative, but the right upper quadrant is equivocal.
At this point, her pressure drops again. You re-evaluate your ABCs and find nothing new. The femurs appear to be nicely reduced, and the thighs are not larger than they were when she arrived. Your surgeon is concerned that the abdomen may be the source despite the (mostly) negative FAST. Due to BP concerns, she proceeds to do a DPL.
The procedure proceeds smoothly while resuscitation with blood products takes place. There is no gross blood on the tap. A liter of saline is infused and is now freely emptying into a bag. For the first 400cc, the effluent is crystal clear. But now you start to see something.

Hmm, is it or isn’t it? Let’s take a closer look.
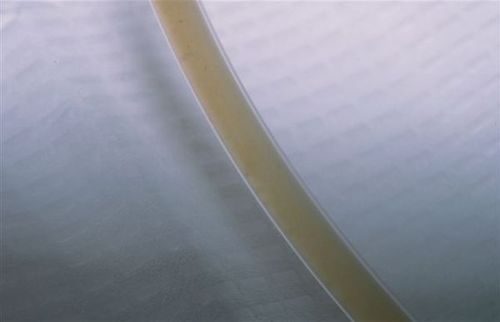
Yeah, that’s weird. Just of hint of some kind of tiny darkish particles settling to the bottom of the tubing. Hmmm!
So what’s happening here? And what should you do? More information tomorrow. Please comment or tweet your guesses!