Yesterday, I outlined the AAST organ injury scale for the pancreas. Today, I’ll go through diagnosis of the the injury in adults.
First, there are two ways of detecting this injury. In stable patients, it is usually identified on CT. Hematoma around an area of the pancreas, combined with linear changes in the density of the gland are typical. It may be difficult to detect in very thin patients without a lot of contrasting fat (although this situation is becoming very uncommon). And obviously, CT is only to be used for stable patients.

The other way this injury is discovered is in the OR during the trauma exploration. This is the most common situation in patients taken directly to OR due to hemodynamic status.
Even if the diagnosis has been made by CT, the diagnostic process continues in the OR. So in all cases, the usual approach to trauma laparotomy applies (large midline incision, control of hemorrhage, control of contamination in that order). Only then can a full inspection be carried out, and damage control principles should be followed. If a pancreatic injury is suspected but the laparotomy must be terminated for damage control reasons, a simple drain should be placed over the pancreas, and the injury addressed on the first takeback.
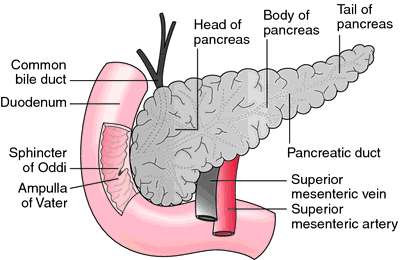
The two keys to deciding what to do in pancreatic injury are injury grade and duct status, which go hand in hand. Sometimes it is difficult to evaluate the duct and there are two ways to approach this in the OR: extra-ductal and intra-ductal. The former is the easiest, and involves direct inspection of the gland. Careful, gentle dissection coupled with close review with magnification will frequently show obvious leakage of clear fluid. The latter involves injecting contrast into the duct. This can be accomplished via either end of the pancreas (directly into the papilla via duodenotomy, into the distal end via distal pancreatectomy), or through on-table ERCP. Neither of the invasive methods are for the faint of heart, and will be discussed in future blog posts. And ERCP can be challenging because patient positioning with an open abdomen is difficult.
Once the grade and duct status have been identified, it’s time to think about fixing the problem. That’s the topic for tomorrow.
Related posts: