There’s a lot of dogma in trauma care, as well as in the field of medicine generally. The knee dislocation dogma is that the incidence of vascular injury is high (around 50%) with posterior dislocation and somewhat lower with non-posterior dislocation.
At least, that’s what I learned way back when. After recently finding myself spouting off those numbers, I wondered if it was really true. Our diagnostic imaging and vascular care have increased considerably in the last few decades, so I decided to check it out.
This lovely image from EMDocs.net shows the various dislocation types. It also gives you an idea of why an associated vascular or nervous injury is so common.
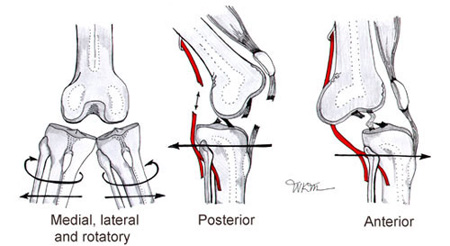
(The nomenclature of the dislocation is based on the direction in which the tibia and fibula move with respect to the femur.)
The orthopedic surgery group at UCLA performed a meta-analysis of the literature on knee dislocation complications. They identified seven papers describing the injuries of 862 patients.
Here are the factoids:
- The overall incidence of vascular injury with knee dislocation was 18%, and nerve injury was 25%
- The incidence of vascular injury with the various types of dislocation was:
- Posterior dislocation: 25%
- Anterior dislocation: 19%
- Lateral dislocation: 18%
- Medial dislocation: 7%
- Rotatory: 14%
- Disruption of both cruciate ligaments as well as the lateral or medial collateral ligament had a very high incidence of vascular injury (32% and 26% respectively)
- About 80% underwent surgical repair of the popliteal artery, but the amputation rate was 12%(!)
Bottom line: The old dogma regarding vascular injury after knee dislocation may be slightly exaggerated. However, it is still common after knee dislocation and can lead to devastating complications.
If your patient tells you that they felt a popping sensation in their knee or have a mechanism consistent with knee dislocation (e.g., pedestrian struck), be very suspicious for this injury. A thorough yet gentle exam, including good neurologic and vascular exams, should be performed. Calculating the Arterial Pressure Index (API) may be helpful but will not keep you from obtaining imaging studies. Multi-plane knee imaging is required, and a CT angiogram/runoff study should be performed to exclude a vascular problem.
Reference: Vascular and Nerve Injury After Knee Dislocation: A Systematic Review. Clin Orthop Relat Res 472(9):2621-9, 2014.




