Yes, more on predictions. We all know that chest trauma is one of the bigger causes of morbidity and mortality in trauma patients. A number of methods have been developed to predict which patients might deteriorate after sustaining chest injury, and where to place them in the hospital on admission. Elderly patients are at particular risk, and determining who to look after more closely, and/or in the intensive care unit, can be very helpful.
The authors of this abstract from West Virginia University took a slightly different approach. Let’s say we have already placed a patient in a ward bed after admission for rib fractures. How can we monitor them and preemptively increase interventions or move to the ICU before they crash and burn?
The WVU group developed a rib fracture guideline nearly 10 years ago, and retrospectively reviewed their experience with 1106 patients over a 6 year period. They measured serial forced vital capacity readings in these patients, and arbitrarily used thresholds of <1, 1-1.5, and >1.5 to predict deterioration.
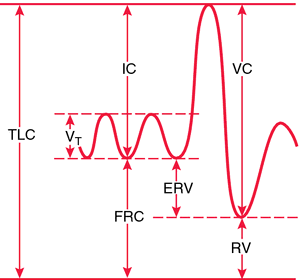
To boost your memory, look at the following chart. The vital capacity is the maximum amount of volume that can be voluntarily exhaled.
Here are the factoids:
- Only patients with initial FVC > 1 were enrolled in the study
- They were then separated into two groups: those whose FVC remained greater than 1 (83%), and those in whom it decreased below 1 (17%)
- Patients in the low FVC group had significantly more complications like pneumonia, intubation, or unplanned transfer to ICU (15% vs 3%) and a longer length of stay
- However, the low FVC group also had a higher chest AIS score, higher ISS, were 10 years older, and were twice as likely to have COPD
Bottom line: Seems like a promising study, right? Check out an easy to measure, objective test and step up your level of care if it dips below a certain critical value? But not so fast. The two study groups look like they are very different. No significance testing was shown for these differences, but they certainly look like they should be different. Couldn’t their deterioration have been predicted based on their age and degree of chest injury?
Here are some questions for the authors to consider before their presentation:
- Please provide the details of your rib fracture pathway
- Your FVC threshold does not have any units assigned. I am assuming that it is in liters. Please clarify.
- Why did you describe three cohorts initially, then settle on the lowest (FVC < 1) as your final threshold? Was there a method to this? Why not 1.5? Or 0.75?
- Did you do any further analysis to try to determine if the differences between the groups were responsible for the differences in complication rates?
- Big picture question: So why couldn’t you just use a specific age/ISS/comorbidity threshold and predict failure at the time of admission, and forget about measuring several FVC values?
Reference: EAST 2018 Podium paper #9.
