I know what you are saying. Button batteries? Trauma? Not too many adult trauma professionals have seen or heard of this. But those who care for pediatric patients should be very familiar. If the importance of this seemingly minor problem is ignored, the results can be catastrophic.
Kids eat stuff, and not just food. The smaller ones always seem to be putting things in their mouths. Foreign body ingestion (or insertion into other orifices) is a common presentation at pediatric emergency departments. Unfortunately, the fact that a battery has been eaten may not be appreciated by the parents. The child may be brought in with nonspecific GI or respiratory symptoms.
As soon as a battery ingestion is known or suspected, a two-view chest x-ray is needed. This should show both chest and upper abdomen in order to visualize both esophagus and stomach. Separate chest and abdominal images may be required if the child is too large for a single shot. Two views (AP and lateral) are important because the nature of the foreign body may not be appreciated if the battery is seen edge-on.
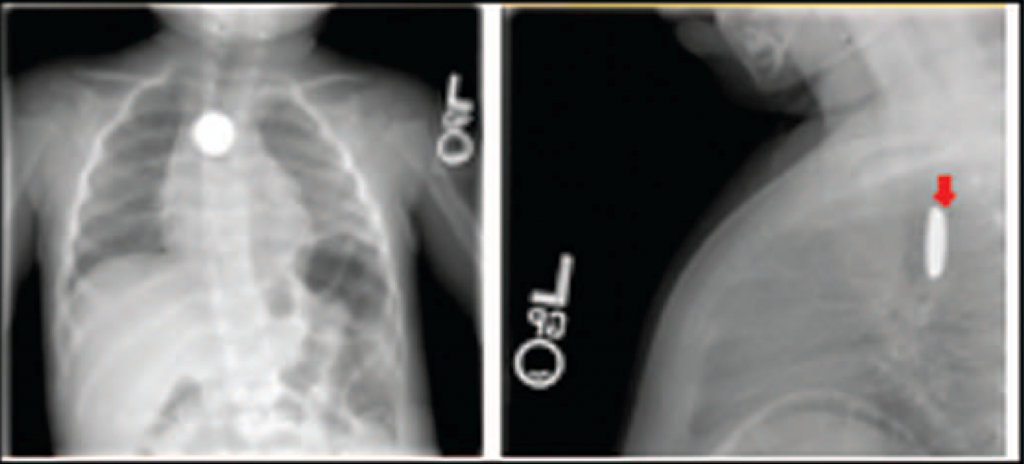
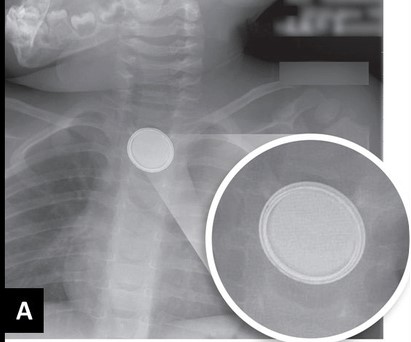
If you are fortunate enough to image the battery “face-on”, you may see a telltale halo sign. Because of the way these batteries are put together, there are two metal sides that have a slight difference in overlap.
You’ve made the diagnosis! So now what? And how quickly? I’ll deal with this in my next post.

