TBI is a very common injury, and neurosurgeons are relatively rare resources for trauma centers. That mismatch can create significant problems for trauma programs. Reflexively, we consult neurosurgeons for a wide variety of neurotrauma, ranging from the very severe to the extremely mild.
Can we intelligently and selectively utilize the skills of our neurosurgeons, and not jeopardize patient safety? Surgeons at Baystate Medical Center in Springfield MA reviewed their own experience managing mild TBI.
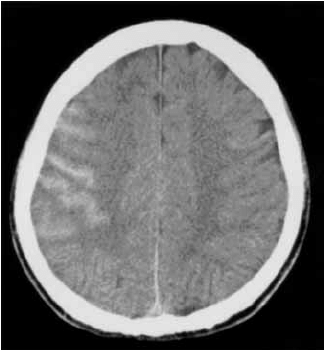
They defined a mild TBI as one with patient GCS of 13-15. However, their study included only patients with “GCS>14”, which I presume means all patients with GCS=15 (unless this is a typo). They allowed patients with normal GCS and intoxication, epidural (EDH) or subdural hematoma (SDH)<4mm, small subarachnoid hemorrhage (SAH), and non-displaced skull fracture (Fx). Any patient taking any type of anticoagulant or anti-platelet drug was excluded. They looked at need for neurosurgical consultation or intervention, readmission, and 30 day mortality.
This prospective study spanned 13 months. This lower volume center admitted 1341 patients, of which 77 were included in the study. Average age was 55, and average ISS was 16. A total of 97% presented for a followup visit (!).
Here are the factoids:
- 47% had SAH, 43% SDH, 16% intraparenchymal hemorrhage (not mentioned in inclusion criteria), 14% Fx, and no EDH
- Only one patient required neurosurgery consult, and none required intervention
- There were no mortalities
- Most (62%) were admitted to a ward bed, and the average length of stay for all patients was 3 days
- Cost savings was estimated at about $16,000
Bottom line: Yes there is no magic in getting a neurosurgical consult for most mild TBI. The study is small, but telling. A carefully crafted practice guideline can dramatically decrease the (over)use of our neurosurgeons, saving both time and money.
In reviewing their guideline, I would recommend shaving even one more point off the GCS (>14), but stipulating that any central subarachnoid hemorrhage require consultation because of the possibility of an aneurysm being the culprit.
Check out the guideline in use at my hospital below. Also, look at the first related post, which is similar in idea to this one, but you can see the difference in management by surgeons vs neurosurgeons.
Related posts:
- Can TBI be managed without neurosurgical consultation?
- Placement of ICP monitors by non-neurosurgeons
- Practice guideline for TBI management without neurosurgeons
Reference: Mild traumatic brain injuries can be safely managed without neurosurgical consultation: the end of a neurosurgical “nonsult”? AAST 2016, Poster 51.

