This is an 8 minute tutorial on the extended FAST exam (eFAST). Nice visualizations on an enthusiastic medical student. This was originally presented at Trauma Education: The Next Generation in September 2013.
Monthly Archives: July 2014
Here’s a quick and dirty video on how to use a needle (a really big one) to decompress the chest. Piece of cake!
WTF? A Fractured Rudimentary Rib?
Is it real, or just another one of those crazy things that radiologists like to add to their reports? I recently came across one of these for the first time in over 30 years of practice. What is it? And is it significant in your management of a trauma patient?
A rudimentary rib is simply an extra one (supernumerary). They can be found on vertebrae where ribs are not supposed to be present, typically C7 and L1. The most common supernumerary ribs are found at C7, and are a well documented cause of thoracic outlet syndrome.
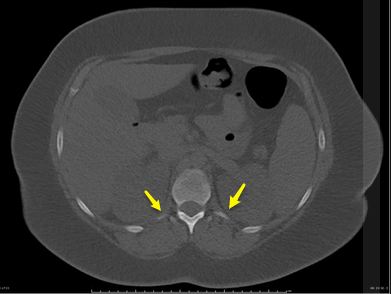
Rudimentary ribs are less commonly found on lumbar vertebrae, and they tend to be longer than the transverse processes. This means that it is possible to break them given moderate to high energy blunt torso trauma. The image below shows a person with 2 rudimentary lumbar ribs on L1.
These are very rare congenital variants. It is more likely that your patient is showing abnormal bone formation after a previous fracture, so question them closely for a history of trauma.
What’s the clinical significance? There’s little chance of hemothorax or pneumothorax. But they cause pain like any other fracture. Just apply your usual routine for rib fracture management: analgesia and pulmonary toilet. Since it takes a relatively large amount of energy to break these short little ribs, be on the lookout for other occult injuries as well.
Bottom line: This isn’t just a weird radiology “red herring.” Rudimentary rib fractures can occur, although a history of previous injury should be ruled out. Manage like any other rib fracture, but beware of potential occult injuries.
Related posts:
The Contaminated Patient
In my last post, I presented the issue of dealing with a surprise patient who was both in arrest and contaminated with gasoline. They are brought into your resuscitation room without warning of the potential hazard. Now that they are here, what do you do?
Thanks for the many online and email responses. This is a tough question, because there are so many variables to think about. And you have to make decisions very quickly. Here’s a rundown on my thought processes.
First, if you get an indication that there might be any type of contamination, insist that your prehospital providers hold the patient outside the ED. Have part of your trauma team waiting at the ambulance dock to do a quick assessment there. Another minute or two of Lucas CPR will not make a difference. Use your best judgment as to how much of a hazard is posed by the fuel/mystery liquid/white powder. But err on the side of being conservative so you don’t end up shutting your entire ED down due to contamination. If in doubt, immediately move to your decontamination area.
If the patient ends up deep in your ED before anyone recognizes that there might be a contamination problem, you must heed three overarching principles:
- Limit contamination to the rest of your facility. Close the doors to the resuscitation room. Notify security and your hazardous materials team so they can start working on containment and safety issues outside the room. Failure to do this can take your entire hospital offline. If the situation turns out to be a multiple or mass casualty event and your hospital was the only one able to respond, you’ve just created a catastrophe and delayed treatment for the other patients.
- Ensure the safety of your team. This is a great reason to require and enforce that everyone on the team dress up completely for every resuscitation. You never know where your patients have been, and when one of these will sneak in.
- Continuously assess the risk:benefit ratio. Is the contamination a minor irritant? What is the danger to the team? The ED/hospital? How likely are your efforts to save the patient to succeed? As soon as the ratio goes bad, rethink the options and act accordingly.

Bottom line: In situations like this, think fast and think globally. Don’t just consider the patient. There may be many more lives at stake, and this can and should factor into your decisions about where and how long to continue resuscitation.
In this case, we were certain it was only gasoline. We closed the doors and quickly stripped the patient, bagging the clothes tightly. We tried not to generate any sparks, but we are surrounded by all kinds of electrical equipment. Defibrillation was out of the question. After the event was finished, it was time to wash everything down and start thinking about what would have happened if this had been something more toxic than fuel!
Related post:
What Would You Do? The Contaminated Patient
Here’s some food for thought. Read through the scenario below, as well as the questions under it. I’m interested in some comments from prehospital providers, physicians and nurses in the ED on what you would do in this situation.
Scenario: Paramedics call ahead to activate your trauma team for a young male who was ejected from his car during a motor vehicle crash. He was quickly extricated and was found to be in pulseless electrical activity (PEA) arrest. IVs were inserted and the Lucas automated CPR device was attached. The patient is immobilized and will arrive at your hospital in 5 minutes.
You assemble your trauma team and are patiently awaiting when the medics arrive. The patient / Lucas / backboard are rapidly transferred over to the ED stretcher and mechanical CPR continues. At that point, you are overwhelmed by the odor of gasoline, and you note that the patient’s clothing is saturated with liquid.
What would you do? 
Here are my questions for you:
- Do you move the patient or keep him in your trauma bay?
- What if your decontamination area is a short/moderate/longer distance from your ED?
- What if this situation involved a farmer in arrest who smelled strongly of pesticide? Any different?
- Or someone covered with mysterious white powder?
- How do you balance patient survival and team safety?
- What kind of performance improvement activities will be needed with regard to the team? The prehospital providers?
This discussion is not suited to the 140 character limitation of Twitter, so please click the Comments link below and let me know what you think. I’ll give my take on this next week.
