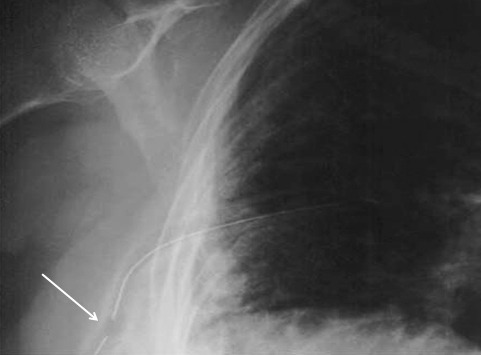
Yesterday I presented the problem of the malpositioned chest tube, specifically one that is not completely in the pleural space. This one is way out:
So what do the doctor books say? Well, the first thing you will discover if you try to look it up is that THERE IS NO LITERATURE ON THIS COMMON PROBLEM! There are a few papers on tubes placed in the fissure and tubes inserted into the lung parenchyma. But there are only a few mentions of tubes with holes still outside the chest.
I’ve gotten a number of comments, including “you can push them in a little”, “take it out and put in another”, and “never push them in.” Since we don’t have any science to guide us, we have to use common sense. But remember, I’ve shown you plenty of examples where something seems reasonable, but turns out to be ineffective or downright harmful.
There are three principles that guide me when I face this problem:
- Prevention is preferable to intervention
- Do no (or as little as possible) further harm
- Be creative
Monday, I’ll finish this series and provide some tips and guidelines to help manage this problem using the principles outlined above.