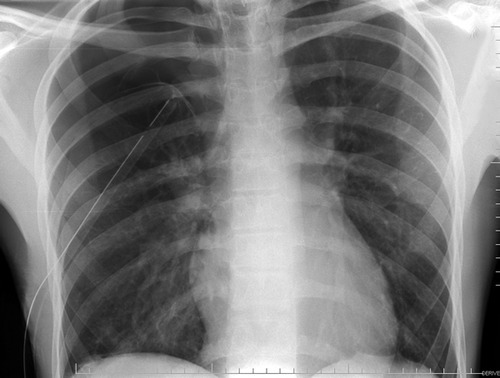
I showed you this x-ray the other day, and asked what the problem was.
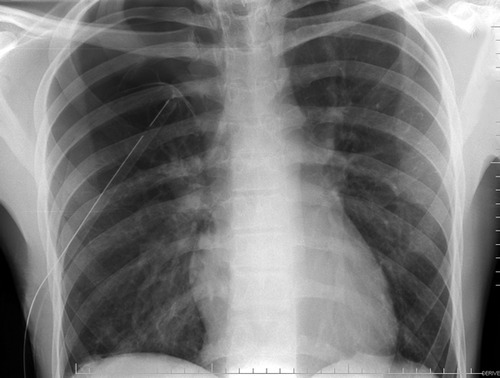
If you look carefully, you can see the lung outline in the middle of the right side of the chest. Big-time pneumothorax despite what looks like a perfectly placed tube. There are several possible explanations, and many of you sent me your guesses:
- The tube is in the lung. This rarely happens to normal lungs. Sure, you can probably do it to an ARDS lung, but otherwise it’s not likely.
- The tube is in the fissure. This does happen on occasion, but not often. And many times it works anyway.
- The tube is occluded or kinked. A PA or AP chest x-ray will show the kink, although bent tubes frequently work anyway. If a hemothorax is present, it is possible that a clot is plugging the tube. Clearing a plugged tube will be the subject of another post.
- It’s not really a chest tube. Hopefully, this would have been detected when it was placed, but it’s not always. The chest x-ray above looks great, right? Unfortunately, it’s a 2 dimensional representation of a 3-D object. Where is that tube in the z-axis?
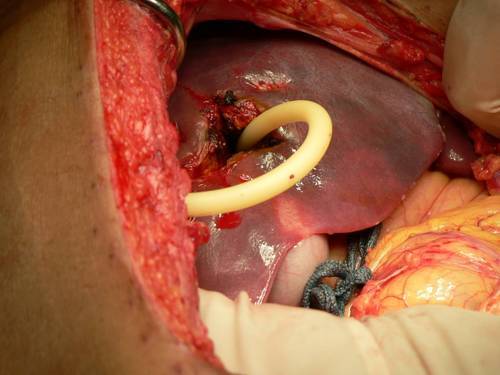
In this case the correct answer is the last one. This is one time when I would actually recommend a lateral chest x-ray. Have a look at the result. You can clearly see the tube snaking around into the soft tissues of the back.
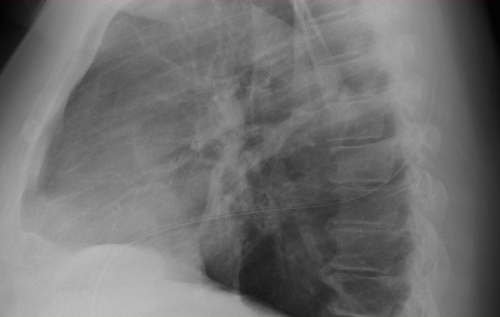
Bottom line: Remember that a perfect x-ray doesn’t necessarily mean a perfect tube. Go through the various possibilities quickly, and make it work.
Related posts: