I recently read a very interesting article on research, and found it to be very pertinent to the state of academic research today. It was published on Manager Mint, a site that considers itself to be “the most valuable business resource.” (?) But the message is very applicable to trauma professionals, medical professionals, and probably anyone else who engages in research pursuits. The link to the full article is listed at the end of this post.
1. Research is not good because it is true, but because it is interesting.
Interesting research doesn’t just restate what is already known. It creates or explores new territory. Don’t just read and believe existing dogma.
Critique it.
Question it. Then devise a way to see if it’s really true.
2. Good research is innovative.
Some of the best ideas come from combining ideas from various disciplines.
Some of the best research ideas are derived from applying concepts from totally unrelated fields to your own.
That’s why I read so many journals, blogs, and newsfeeds from many different fields. And even if you are not doing the research, a broad background can help you sort out and gain perspective as you read the works of others.
3. Good research is useful.
Yes, basic bench level research can potentially be helpful in understanding all the nuances of a particular biochemical or disease process.But a lot of the time, it just demonstrates relatively unimportant chemical or biological reactions. And only a very small number actually contribute to the big picture. For most of us working at a macro level, research that could actually change our practice or policies is really what we need.
4. The best research should be empirically derived.
It shouldn’t rely on complicated statistical models. If it does, it means that the effect being measured is very subtle, and potentially not clinically significant. There is a big difference between statistical and clinical relevance.
Reference: If You Can’t Answer “Yes” To These 5 Questions, Your Research Is Rubbish. Garrett Stone. Click here to view on Manager Mint.

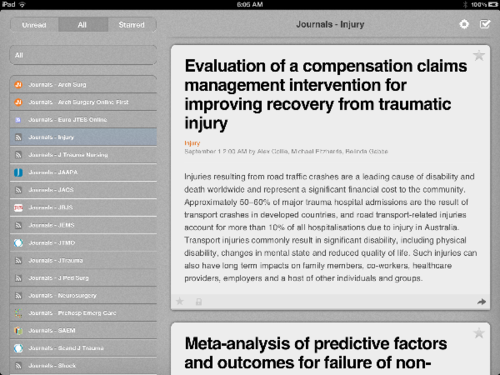
 icons on web pages. There are loads of RSS readers available, both online and for handheld devices, that allow you to organize and browse content from RSS feeds. I use Google Reader on desktops or laptops, and the River of News app on my iPad.
icons on web pages. There are loads of RSS readers available, both online and for handheld devices, that allow you to organize and browse content from RSS feeds. I use Google Reader on desktops or laptops, and the River of News app on my iPad.