Over a year ago I published a series on using the hybrid room for trauma cases. In the meantime, some new papers have been published on this concept. Over the next two weeks, I’ll be refreshing and republishing this information to help you optimize the use of yours, or to support your efforts to get one if you don’t.
While quite a bit of trauma care is routine, involving simpler, single system injuries, a small subset of our patients sustains major, multi-system, and life-threatening ones. They require rapid access to skilled trauma professionals and advanced resources including imaging, operating rooms, and other procedures.
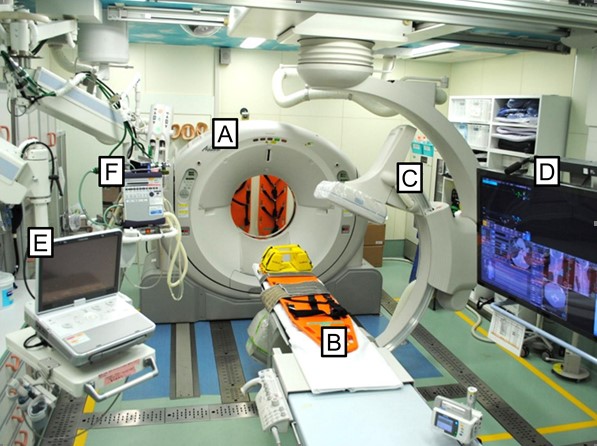
In most trauma centers, initial resuscitation takes place in a trauma resuscitation room in or near the ED. Some diagnostic imaging can be performed there, but more sophisticated studies may require a short (or longer) road trip. Operating rooms and other procedural areas are also usually more distant. And most importantly, each of these areas is designed for a single discipline. Diagnostic radiology has equipment, technicians, and radiologists available. Interventional radiology contains the specialized equipment needed for this more invasive procedure. ORs are designed specifically for surgical procedures, and frequently contain equipment for a single surgical discipline.
But some of our patients require it all! Think about a patient who arrives after a major car crash. Blood pressures are soft, the pelvis is grossly unstable, FAST exam is positive, and there is bleeding from the vagina.
How do we prioritize? Where do we go first? How long will it take the interventional radiology team to arrive? Where’s that external fixator equipment? Can we slip in a CT scan? Where’s OB/GYN??
The solution is right under our nose! Many hospitals have added so-called “hybrid ORs” to their operating suites in order to address the needs of their vascular and cardiovascular surgeons. The next several posts will cover everything you need to know about this important tool for trauma care. I’ll review:
- What is a hybrid OR, exactly?
- Why use a hybrid OR for trauma?
- Is the hybrid OR for trauma useful?
- Which patients may benefit from a hybrid OR?
- So you want your own hybrid room?!
Next post: what is a hybrid OR, exactly?