In my last post I reviewed several older papers that showed some positive associations with the use of a hybrid room for trauma patients. However, these rooms were not dedicated to the trauma patient. This means that they may not be staffed at all hours, or other elective cases could be scheduled in them. In either case, there were periods of time where the hybrid room might not be available for trauma procedures.
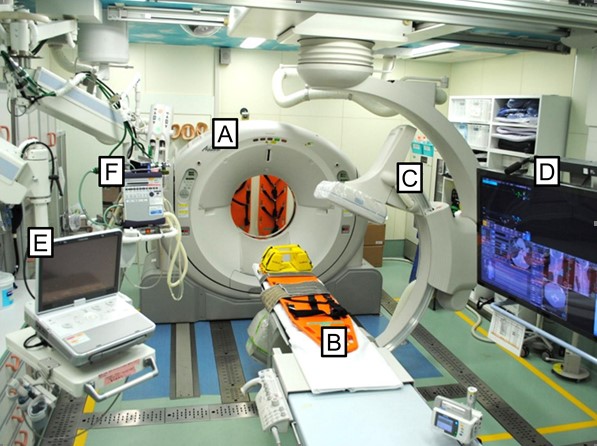
A study of the experience of one trauma center (University of Florida, Gainsville) with a truly dedicated, always available hybrid room for trauma patients was published just last month. Three and a half years of experience with the room was compared with historical controls from a similar period of time before implementation. Patients younger than 18 were excluded, as were patients operated for reasons other than bleeding control (i.e. emergent trach). The room itself was a repurposed and remodeled angiography suite located one floor above the emergency department trauma bays.
Here are the factoids:
- Overall patient demographics, including mechanism, severity of injury, prehospital intubation, and initial blood pressure.
- Median Injury Severity Score (ISS) was 18 pre-hybrid and 22 post (not statistically significant but probably clinically so)
- There was greater use of REBOA in the post-hybrid group (8%) vs pre-hybrid OR (1%)
- The hybrid group achieved earlier hemorrhage control (49 vs 60 minutes); this is both statistically and clinically significant!
- Blood and plasma transfusions given between 0 and 4 hours of arrival were the same pre- vs post-hybrid (3 vs 2.5 units PRBC and 2 vs 1.5 units plasma)
- Although the authors claim significantly fewer transfusions of both products between 4 and 24 hours, the numbers are clinically the same (1 vs 0 units of each)
- The number of infectious complications was significantly less (27% pre- vs 15% post), but was entirely driven by pneumonia reduction from 12% to 4%. All other infections (bloodstream, surgical site, UTI, C. Diff, graft infection) were the same.
- The number of days on the ventilator decreased from 3 to 2, which was statistically significant but clinically questionable
Bottom line: This paper was a bit problematic for me. I want to believe that a hybrid room is valuable because I’ve been involved with a handful of cases where I believe it made a big difference. And if you read only the abstract or the conclusions of the paper, it sounds great!
Always be careful of papers that go along with your confirmation bias. Read them even more carefully than you normally would. I have a few comments / questions:
- First, the good news. The time to hemorrhage control decreased from 60 to 49 minutes using the hybrid room. Eleven minutes. Doesn’t seem like a lot, but this is probably the most important conclusion. Ongoing bleeding rapidly decreases survival, and literally, every minute counts.
- Why was so little blood and plasma given? I can’t recall a hybrid room case where we have given less than 10 units of blood and other products. The volumes given in this study were just a couple of units, and the decrease of half a unit was statistically significant. In my opinion, this is not clinically relevant in these sick patients. But this fact is touted in the abstract and conclusion. And you can’t chalk it up to REBOA, because they only used it in 8% of the hybrid room patients.
- The decrease in pneumonia was indeed clinically significant, dropping from 27% to 15%. However, all other infectious complications remained the same. But once again, the fact that infections (generically) were significantly decreased was called out in the abstract and conclusions. Just focus on pneumonia because that’s all it was.
- Ventilator days decreased from 3 to 2 days, which may or may not be clinically significant even though statistical significance was achieved. This, too, is emphasized in the abstract and conclusions.
I really wanted this to paper to soundly demonstrate how great a dedicated hybrid room is. But what I see is a single-center experience that only shows that it clinically significantly decreases time to hemorrhage control and the incidence of pneumonia and not much more. The authors hit the nail on the head with their last sentence:
Association between time to hemorrhage control and clinical outcomes require further investigation, ideally using granular, standardized electronic health record data from multiple institutions.
I will keep waiting for the next paper and hope it really answers these questions! This one left me wanting a lot more.
Reference: Clinical impact of a dedicated trauma hybrid operating room. JACS 232(4):560-571, 2021.