Does Initial Hematocrit Predict Shock?
Everything you know is WRONG!
The classic textbook teaching is that trauma patients bleed whole blood. And that if you measure the hematocrit (or hemoglobin) on arrival, it will approximate their baseline value because not enough time has passed for equilibration and hemodilution. As I’ve said before, you’ve got to be willing to question dogma!
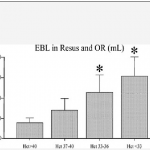
The trauma group at Ryder in Miami took a good look at this assumption. They drew initial labs on all patients requiring emergency surgery within 4 hours of presentation to the trauma center. They also estimated blood loss in the resuscitation room and OR and compared it to the initial hematocrit. They also compared the hematocrit to the amount of crystalloid and blood transfused in those areas.
Patients with lower initial hematocrits had significantly higher blood loss and fluid and blood replacement during the initial treatment period. Some of this effect may be due to the fact that blood loss was underestimated, or that prehospital IV fluids diluted the patient’s blood counts. However, this study appears sound and should prompt us to question the “facts” we hear every day.
Bottom line: Starling was right! Fluid shifts occur rapidly, and initial hematocrit or hemoglobin may very well reflect the volume status of patients who are bleeding rapidly. If the blood counts you obtain in the resuscitation room come back low, believe it! You must presume your patient is bleeding to death until proven otherwise.
Reference: Initial hematocrit in trauma: A paradigm shift? J Trauma 72(1):54-60, 2012.