Autotransfusing blood that has been shed from the chest tube is an easy way to resuscitate trauma patients with significant hemorrhage from the chest. Plus, it’s usually not contaminated from bowel injury and it doesn’t need any fancy equipment to prepare it for infusion.
It looks like fresh whole blood in the collection system. But is it? A prospective study of 22 patients was carried out to answer this question. A blood sample from the collection system of trauma patients with more than 50 cc of blood loss in 4 hours was analyzed for hematology, electrolyte and coagulation profiles.
The authors found that:
- The hemoglobin and hematocrit from the chest tube were lower than venous blood (Hgb by about 2 grams, Hct by 7.5%)
- Platelet count was very low in chest tube blood
- Potassium was higher (4.9 mmol/L), but not dangerously so
- INR, PTT, TT, Factor V and fibrinogen were unmeasurable
Bottom line: Although shed blood from the chest looks like whole blood, it’s missing key coagulation factors and will not clot. Reinfusing it will boost oxygen carrying capacity, but it won’t help with clotting. You may use it as part of your massive transfusion protocol, but don’t forget to give plasma and platelets according to protocol. This also explains why you don’t need to add an anticoagulant to the autotransfusion unit prior to collecting or giving the shed blood!
Reference: Autotransfusion of hemothorax blood in trauma patients: is it the same as fresh whole blood? Am J Surg 202(6):817-822, 2011.
Autotransfusing blood that has been shed from the chest tube is an easy way to resuscitate trauma patients with significant hemorrhage from the chest. Plus, it’s usually not contaminated from bowel injury and it doesn’t need any fancy equipment to prepare it for infusion.
It looks like fresh whole blood in the collection system. But is it? A prospective study of 22 patients was carried out to answer this question. A blood sample from the collection system of trauma patients with more than 50 cc of blood loss in 4 hours was analyzed for hematology, electrolyte and coagulation profiles.
The authors found that:
- The hemoglobin and hematocrit from the chest tube were lower than venous blood (Hgb by about 2 grams, Hct by 7.5%)
- Platelet count was very low in chest tube blood
- Potassium was higher (4.9 mmol/L), but not dangerously so
- INR, PTT, TT, Factor V and fibrinogen were unmeasurable
Bottom line: Although shed blood from the chest looks like whole blood, it’s missing key coagulation factors and will not clot. Reinfusing it will boost oxygen carrying capacity, but it won’t help with clotting. You may use it as part of your massive transfusion protocol, but don’t forget to give plasma and platelets according to protocol. This also explains why you don’t need to add an anticoagulant to the autotransfusion unit prior to collecting or giving the shed blood!
Related post: Chest tubes and autotransfusion
Reference: Autotransfusion of hemothorax blood in trauma patients: is it the same as fresh whole blood? Am J Surg 202(6):817-822, 2011.
Autotransfusing blood that has been shed from the chest tube is an easy way to resuscitate trauma patients with significant hemorrhage from the chest. Plus, it’s usually not contaminated from bowel injury and it doesn’t need any fancy equipment to prepare it for infusion.
It looks like fresh whole blood in the collection system. But is it? A prospective study of 22 patients was carried out to answer this question. A blood sample from the collection system of trauma patients with more than 50 cc of blood loss in 4 hours was analyzed for hematology, electrolyte and coagulation profiles.
The authors found that:
- The hemoglobin and hematocrit from the chest tube were lower than venous blood (Hgb by about 2 grams, Hct by 7.5%)
- Platelet count was very low in chest tube blood
- Potassium was higher (4.9 mmol/L), but not dangerously so
- INR, PTT, TT, Factor V and fibrinogen were unmeasurable
Bottom line: Although shed blood from the chest looks like whole blood, it’s missing key coagulation factors and will not clot. Reinfusing it will boost oxygen carrying capacity, but it won’t help with clotting. You may use it as part of your massive transfusion protocol, but don’t forget to give plasma and platelets according to protocol. This also explains why you don’t need to add an anticoagulant to the autotransfusion unit prior to collecting or giving the shed blood!
Related post: Chest tubes and autotransfusion
Reference: Autotransfusion of hemothorax blood in trauma patients: is it the same as fresh whole blood? Am J Surg 202(6):817-822, 2011.
Autotransfusing blood that has been shed from the chest tube is an easy way to resuscitate trauma patients with significant hemorrhage from the chest. Plus, it’s usually not contaminated from bowel injury and it doesn’t need any fancy equipment to prepare it for infusion.
It looks like fresh whole blood in the collection system. But is it? A prospective study of 22 patients was carried out to answer this question. A blood sample from the collection system of trauma patients with more than 50 cc of blood loss in 4 hours was analyzed for hematology, electrolyte and coagulation profiles.
The authors found that:
- The hemoglobin and hematocrit from the chest tube were lower than venous blood (Hgb by about 2 grams, Hct by 7.5%)
- Platelet count was very low in chest tube blood
- Potassium was higher (4.9 mmol/L), but not dangerously so
- INR, PTT, TT, Factor V and fibrinogen were unmeasurable
Bottom line: Although shed blood from the chest looks like whole blood, it’s missing key coagulation factors and will not clot. Reinfusing it will boost oxygen carrying capacity, but it won’t help with clotting. You may use it as part of your massive transfusion protocol, but don’t forget to give plasma and platelets according to protocol. This also explains why you don’t need to add an anticoagulant to the autotransfusion unit prior to collecting or giving the shed blood!
Related post: Chest tubes and autotransfusion
Reference: Autotransfusion of hemothorax blood in trauma patients: is it the same as fresh whole blood? Am J Surg 202(6):817-822, 2011.
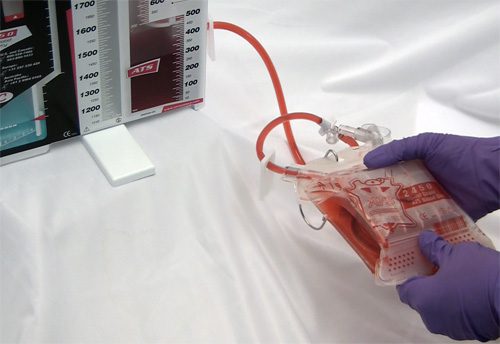
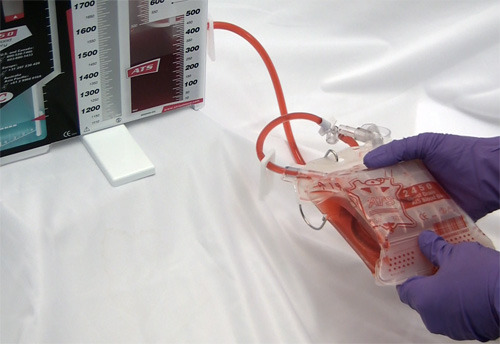
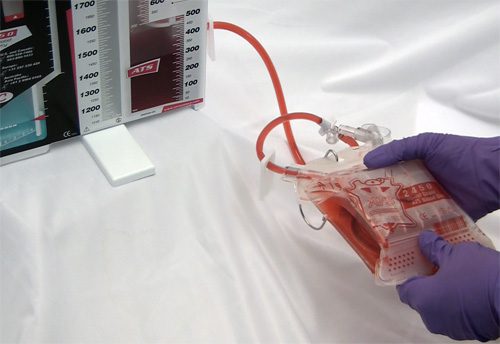
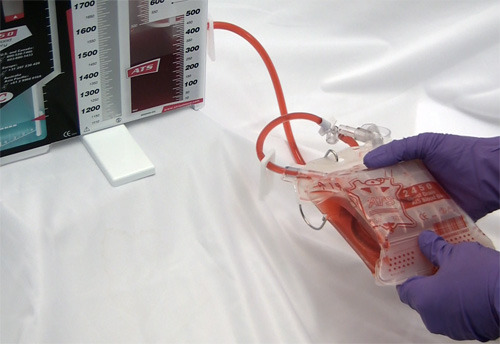
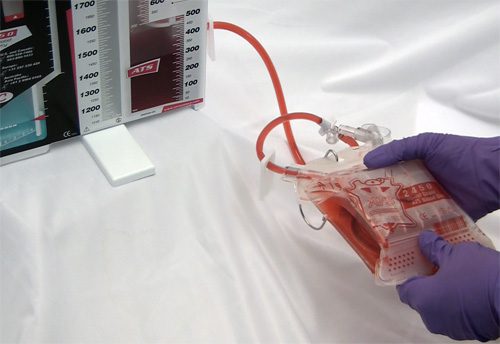
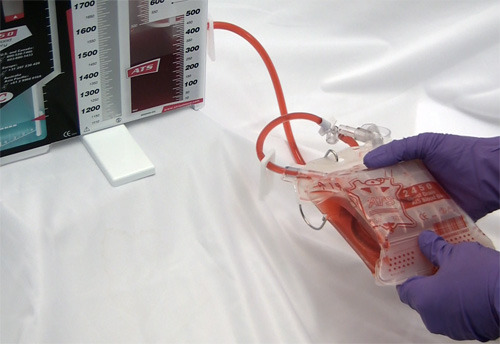
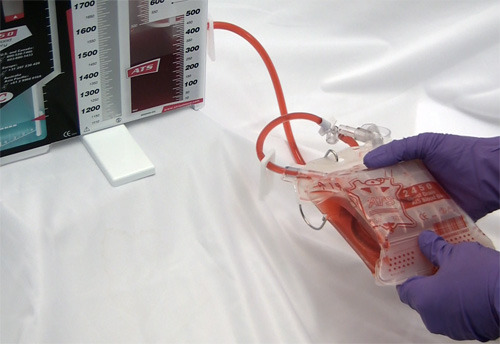
Chest trauma is common in trauma patients. Chest tubes are required with some regularity for the management of hemothorax and/or pneumothorax. Occasionally, the amount of blood in the chest is substantial, and when the tube goes in we wish that we were able to transfuse that blood.
Well, you can! Most collection systems have optional autotransfusion canisters that connect to the chest tube inline with the collection system. The canisters are used to collect shed blood and can then be hung like a bag of blood from the blood bank.
A few key points about using autotransfusion canisters:
- I recommend you consider it for any chest tube being inserted for trauma. They will almost always have some blood in their chest.
- If you want to limit use further due to the expense, just add it for trauma activation patients.
- Always add it to the chest tube collection system before the chest tube goes in. Most of the blood will be lost if the chest tube is hooked to the collection system first.
- No need to anticoagulate the blood. Most systems can be used to reinfuse shed blood up to 6 hours after collection without heparin or other products.
- Be sure to use an inline blood filter. There will be some debris and clumps that must be removed.
- Don’t use the blood if it is likely to be contaminated. This most often occurs with penetrating trauma, where a stab or gunshot could injure stomach or colon and violate the diaphragm.
- Follow the manufacturer’s instructions for your brand of collection system.
Here’s a picture of an autotransfuser that attaches to a Pleur-Evac brand system.

Home of the Trauma Professional's Blog