Tension pneumothorax is an uncommon but potentially lethal manifestation of chest injury. An injury to the lung occurs that creates a one-way valve effect, allowing a small amount of air to escape with every breath. Eventually the volume becomes so large as to cause the lung and mediastinum to push toward the other side, with profound hypotension and cardiovascular collapse.
The classic clinical findings are:
- Hypotension
- Decreased or absent breath sounds on the affected side
- Hyperresonance to percussion
- Shift of the trachea away from the affected side
- Distended neck veins
You should never diagnose a tension pneumothorax with a chest xray or CT scan, because the diagnosis is a clinical one and the patient may die while these procedures are carried out. Having said that, here’s one:
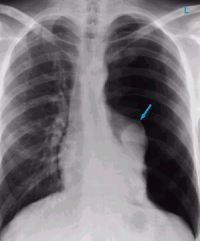
The arrow points to the completely collapsed lung. Note the trachea bowing to the right.
As soon as the diagnosis is made, the right thing to do is to “needle the chest.” A large bore angiocath should be placed in the second intercostal space, mid-clavicular line, sliding right over the top of the third rib. The needle should then be removed, leaving the catheter.
The traditional large bore needle is 14 gauge, but they tend to be short and flimsy. They may not penetrate the pleura in an obese patient, and will probably kink off rapidly. Order the largest, longest angiocath possible and stock them in your trauma resuscitation rooms.

The top catheter in this photo is a 14 gauge 1.25 inch model. The bottom (preferred at Regions) is a 10 gauge 3 inch unit. Big difference!
The final tip to treating a tension pneumothorax is that a chest tube must be placed immediately after inserting the needle. If the patient is on a ventilator, the positive pressure will slowly expand the lung. But if they are breathing spontaneously, the needle will change the tension pneumothorax into a simple open pneumothorax. Patients with other cardiovascular problems will not tolerate this for long and may need to be intubated if you dawdle.
Related post: