Gee, the hybrid OR sounds like a great idea for specific trauma patients. But we’ve seen this before; great idea but doesn’t always translate into a positive result. Is there any literature?
Unfortunately, very little. A group from the University of Calgary in Alberta published a very detailed paper on the nuts and bolts of how they designed their hybrid room from scratch. This paper is very detailed, and the hospital personnel were very thoughtful as they approached the time-consuming and expensive task of designing and building their hybrid room. Of course, they chose a silly acronym as so many do. They called it their RAPTOR room (Resuscitation with Angiography, Percutaneous Treatments, and Operative Resuscitations). Sigh!
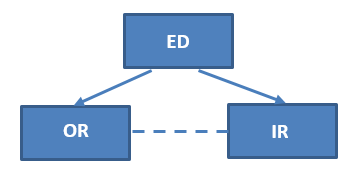
Next, they retrospectively analyzed their experience with persistently hypotensive patients arriving at their Level I trauma center over a 17-year period before their hybrid room opened.
Here are the factoids:
- Of 911 patients, 510 remained persistently hypotensive (SBP<90 torr)
- 53% (270 patients) were taken directly to OR, usually for laparotomy, thoracotomy, or vascular procedure
- 29% were admitted to an ICU, 13% to a ward bed, and 5% were taken to interventional radiology (IR)
- 35 patients (7%) required both OR and IR; the majority had pelvic fractures (77%), the rest had liver lacerations
- Each case was reviewed, and overall 6% of patients would have clearly benefited from a hybrid room, and 30% would have potentially benefited
Sounds good so far! But we need some more data. Unfortunately, there’s not a lot of it yet. A Japanese group described their experience with treating patients in OR then IR, vs a “hybrid procedure.” This did not involve the use of a true hybrid OR. They moved a C-arm fluoroscopy unit into an OR and part of the procedure was carried out by an interventional radiologist.
And the factoids:
- A total of 13 “hybrid treatment” patients were compared to 45 who underwent both operation and angiography, but not in the same location
- Most of the hybrid patients had a laparotomy, but there was a concomitant thoracotomy in one and a craniotomy in another
- The actual survival in the hybrid patients was 85%, while TRISS predicted that only 62% would live
- There was no difference in transfusion volumes between the two groups, but total procedure time was significantly shorter in the hybrid group (4 hours vs 6 hours)
Okay, sounds promising. A second Japanese paper was published last year with much larger numbers. Their hybrid OR was actually a hybrid ER! They installed a multi-slice interventional radiology/CT unit in their resuscitation room! Here are the key findings:
- A total of 696 patients were reviewed over an 8-year period – 336 hybrid and 360 conventional
- Mortality was very significantly decreased in the hybrid group
- OR start was significantly shortened from 68 minutes to 47
Here’s an image of their setup:
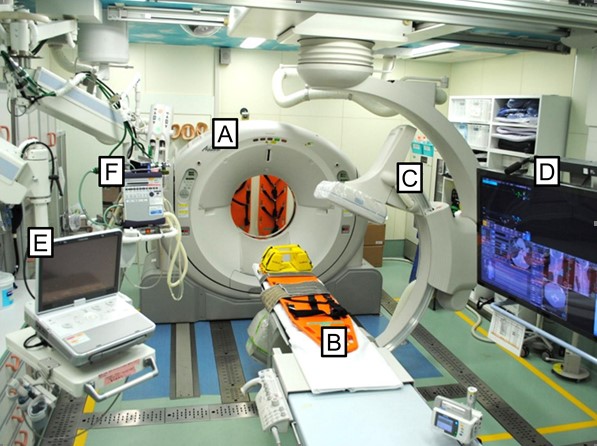
Key: A – mobile CT scanner, B – CT / OR table, C – mobile C-arm, D – 56” monitor, E – ultrasound, F- ventilator
Bottom line: This is quite a unique room. Unfortunately, it is not ideal because it is small and cramped. It looks like it would be difficult to fit more than one surgical team in the room. However, the results look good.
We are finally starting to see objective data involving a reasonable number of patients. A minority of trauma programs have a hybrid OR available to them, and the number of patients who would benefit from it is low. But if a patient needs it, this setup can be life-saving. So who are those patients, exactly?
In my next post, I’ll review a very new (2020) paper specifically on the hybrid room for trauma.
References:
- The evolution of a purpose designed hybrid trauma operating room from the trauma service perspective: The RAPTOR (resuscitation with angiography percutaneous treatments and operative resuscitations). Injury 45:1413-1421, 2014.
- The potential benefit of a hybrid operating environment among severely injured patients with persistent hemorrhage: How often could we get it right? J Trauma 80(3):457-460, 2016.
- Hybrid treatment combining emergency surgery and intraoperative interventional radiology for severe trauma. Injury 47:59-63, 2016.
- The Survival Benefit of a Novel Trauma Workflow that Includes Immediate Whole-body Computed Tomography, Surgery, and Interventional Radiology, All in One Trauma Resuscitation Room. Ann Surg 269(2):370-376, 2019.