It has long been known that blood transfusion decreases immunocompetency for a period of time. This has been taken advantage of in transplant surgery for decades. And blood transfusions are used liberally in major trauma. So could blood transfusion make it more likely for a trauma patient to suffer complications such as pneumonia, sepsis, and surgical site infections?
The group at the Massachusetts General Hospital explored this possibility. The analyzed four years of TQIP data, examining patients who received blood transfusions within four hours of arrival. They excluded transfers in, patients with incomplete transfusion counts, and those who died within 48 hours.
They focused on pneumonia, sepsis, and surgical site infections and statistically controlled for demographics, comorbidities, injury severity, and surgical/procedural interventions.
Here are the factoids:
- A million patients (!) were reviewed and about 41,000 met study criteria
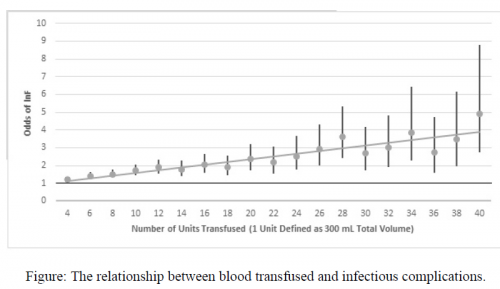
- The odds ratio of infectious complications increased from 1.23 after 2 units to 4.89 after 40 units
- Each additional unit after 40 increased the odds of an infection by another 4.9%
The authors concluded that blood transfusion is associated with a dose dependent risk of infectious complications and that patients should be resuscitated to achieve prompt hemorrhage control (really?).
My comment: Well, this certainly looks fairly straightforward. Of course, it suffers from the usual drawbacks of massaging large databases. And remember, it shows an association, not cause and effect. How can we tease out whether the higher infection risk is due to badly hurt patients who need major surgery and prolonged ICU stays with pneumonia? The authors have tried to reduce this as much as possible using logistic regression. Unfortunately, many of the variables are very interdependent and I don’t believe the methods can fully overcome this. And there may be other factors not available for analysis in the TQIP data.
Here is my only question for the authors and presenter:
-
- How can you be sure that you have fully controlled for the key variables that might influence your final analysis? Yes, you considered demographics, three listed comorbidities (cirrhosis, diabetes, and steroid use), injury severity, and some interventions. But might there be other factors not listed and maybe not even in the TQIP data? Ideas?
This is one of those papers that makes you say “hmm”. But don’t we always try to stop the bleeding promptly. I’m not sure what alternative we have to giving blood.
Reference: Overtransfusion comes at a significant cost: the dose-dependent relationship between blood transfusions and infections after major trauma. EAST Annual Assembly abstract #26, 2020.

