This topic continues to come up from time to time. I still see trauma programs that perform the good, old-fashioned digital rectal exam on nearly every trauma patient. But is it really necessary?
In the not so distant past, it was standard operating procedure to perform a digital rectal exam in all major trauma patients. The belief had always been that valuable information about blood in the GI tract, the status of the urethra, and the neuro exam (rectal tone) could be gleaned from this exam.
Unfortunately, a finger in the bum also serves to antagonize or even further traumatize some patients, especially those who may be intoxicated to some degree. On a number of occasions I have seen calm patients become so agitated by the rectal exam that they required intubation for control.
So is it really necessary? A study in 2001 conducted over a 6 month period (1) showed that the rectal exam influenced management in only 1.2% of cases. The authors felt that there was some utility in 3 special cases:
- Spinal cord injury – looking for sacral sparing
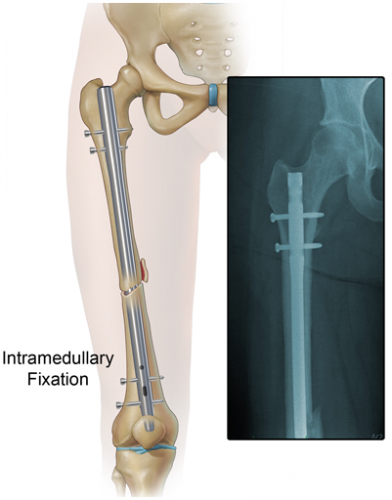
- Pelvic fracture – looking for bone shards protruding into the rectum
- Penetrating abdominal trauma – looking for gross blood
A more recent 2005 study (2) was also critical of the rectal exam and found that using “other clinical indicators” (physical exam and other diagnostic study information) was at least equivalent, changing management only 4% of the time. They concurred with the first two indications above as well.
And what is the best patient position for the exam? I continue to see people try to do it when the patient is in the logroll position! This is substandard for two reasons:
- It is not a stable position, and no one likes a finger in their butt. Awake patients will squirm and withdraw, defeating any attempt at spinal precautions.
- It’s not ideal for the examiner, either. Access to the male prostate is subpar because the examiner’s finger is generally pointed posteriorly, away from this organ. In order to rotate anteriorly, the examiner must spin around, putting “reverse English” (billiards reference) on their arm.
To do a proper rectal exam when indicated, make sure the patient is supine, warn them that you are going to do it, and use the same hand as the side of the patient you are standing on. Right side, right hand to avoid the “reverse English” thing again.
Bottom line: For most major trauma patients, the rectal exam is not worth the patient aggravation it causes. I still recommend it for the 3 special cases listed above, however, as there are no equivalent and effective exams for these potentially serious patient problems. And remember, DON’T do it while the patient is in the logroll position.
References:
1. Porter, Urcic. Am Surg. 2001 May;67(5):438-41.
2. Esposito et al. J Trauma. 2005 Dec;59(6):1314-9.