This 10 minute video was developed with prehospital providers in mind, but all trauma professionals will find some tidbits of interest.
Pay no attention to the hideous screenshot, though. I was not trying to look like House.
This 10 minute video was developed with prehospital providers in mind, but all trauma professionals will find some tidbits of interest.
Pay no attention to the hideous screenshot, though. I was not trying to look like House.
Damage control is over 25 years old already! We continue to refine the techniques and closure techniques/devices, and have developed novel ways to speed closure of the abdominal wall in order to avoid pesky hernias. But the process itself is time intensive, and typically several days pass with regular returns to OR until closure is achieved. This is one of the prime areas in which human error can occur, especially with modern service-style coverage of trauma patients.
In the old days, trauma patients were admitted by their surgeon, and that person provided their care nearly continuously until discharge. He or she rounded on them daily, took them back to the OR when needed, and then discharged them.
This is less practical (and desirable) in this day and age. And even if it seems possible, it’s not. No one can be on call 24 hours a day, and provide comprehensive care to every patient, around the clock. Many trauma programs have adopted a “service model”, where patients are admitted to a defined care team and managed by them. The team is led by a surgeon, but that person may change on a weekly (or in some cases nearly daily) basis. I call this the “interchangeable head” model, and to make it work there must be excellent handoffs during any leadership change.
In some cases, a patient may undergo a damage control procedure by one surgeon, but another must do the takeback and possibly the definitive closure. In this case, the handoff is critical! It is paramount that the next surgeon know everything about the first case so that they can perform the correct procedure.
How can this be accomplished? Here are some tips:
Applying these concepts will decrease the possibility of error, as well as the likelihood of any iatrogenic harm to these complex patients.
Last time, I posted summary info for ED thoracotomy on US trauma centers. Here’s a rundown of the answers provided by international respondents. A few duplicates from the same hospitals have been merged into single answers for them. The total number of international centers for the tables below is now 43.
Level of trauma center (or equivalent)
| Level I | 22 |
| Level II | 8 |
| Level III | 6 |
| No level | 7 |
How many ED thoracotomies are performed per year at your hospital?
| A few per year (<6) | 30 |
| About every month (6-15) | 6 |
| A couple of times a month (16-30)4 | 4 |
| About every week (31-52) | 2 |
| Not specified | 1 |
What type of trauma do you perform ED thoracotomy for?
| Both blunt and penetrating | 22 |
| Penetrating | 17 |
| Blunt | 4 |
Do you use a practice guideline for ED thoracotomy?
| Yes | 17 |
| No | 16 |
| I’m not sure | 10 |
Do you use REBOA in your ED?
| No | 32 |
| Yes | 9 |
| I’m not sure | 2 |
And now for the questions you’ve been waiting for!
Who could perform ED thoracotomy at your hospital? (n=149)
| Surgeon | 39 |
| Emergency physician | 25 |
| Surgical resident / fellow | 15 |
| Emergency medicine resident | 7 |
| Intensivist | 1 |
| ED intern / medical officer | 1 |
| No one | 1 |
Who usually performs ED thoracotomy at your hospital? (n=149)
| Surgeon | 32 |
| Emergency physician | 15 |
| Surgical resident / fellow | 9 |
| Emergency medicine resident | 1 |
| Thoracic surgeon on call | 1 |
| Trauma team leader | 1 |
| Never done one | 1 |
Again, thanks for all who submitted their survey answers. Here’s a rundown of the answers provided by US respondents. A few duplicates from the same hospitals have been merged into single answers for them. Total number of US centers for the tables below is 149.
Level of trauma center
| Level I | 83 |
| Level II | 37 |
| Level III | 15 |
| Level IV | 1 |
| Level V | 2 |
| Seeking verification/designation | 1 |
| No level | 10 |
How many ED thoracotomies are performed per year at your hospital?
| A few per year (<6) | 83 |
| About every month (6-15) | 35 |
| A couple of times a month (16-30) | 23 |
| About every week (31-52) | 8 |
What type of trauma do you perform ED thoracotomy for?
| Both blunt and penetrating | 79 |
| Penetrating | 64 |
| Blunt | 5 |
Do you use a practice guideline for ED thoracotomy?
| Yes | 86 |
| No | 47 |
| I’m not sure | 15 |
Do you use REBOA in your ED?
| No | 88 |
| Yes | 58 |
| I’m not sure | 3 |
And now for the questions you’ve been waiting for!
Who could perform ED thoracotomy at your hospital? (n=149)
| Surgeon | 145 | |
| Emergency physician | 109 | |
| Surgical resident / fellow | 93 | |
| Emergency medicine resident | 66 | |
| APP (PA, NP) | 2 | at one Level I and one Level V |
| Family physician | 1 | at one Level V |
| Family medicine resident | 1 | at one Level V |
Who usually performs ED thoracotomy at your hospital? (n=149)
| Surgeon | 115 | |
| Emergency physician | 25 | |
| Surgical resident / fellow | 69 | |
| Emergency medicine resident | 17 | |
| Never done one | 3 | |
| Family physician or family nurse practitioner | 1 | at one Level V |
Who usually performs ED thoracotomy at your hospital? (By trauma center level)
| Level | I (n=83) | II (n=37) | III (n=15) |
| Surgeon | 64 | 35 | 11 |
| Emergency physician | 8 | 3 | 6 |
| Surgical resident | 63 | 4 | 1 |
| Emergency medicine resident | 12 | 1 | 2 |
| No one | 0 | 0 | 1 |
Join me tomorrow when I review the international data!
The data is in!
Thanks to everybody (all 200+ of you) who participated in the ED thoracotomy survey over the past month. I’m currently compiling the results and will post them here over the next two days.
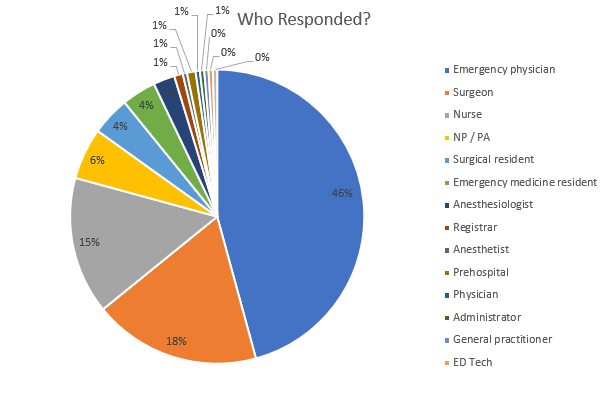
Here is a summary of who responded:
And where were they located?
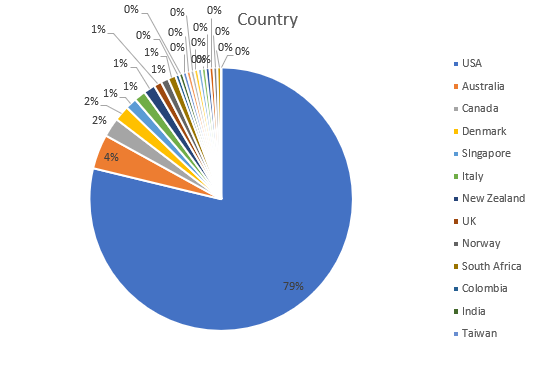
As you can see, the vast majority (167) were from the United States. Australia, Canada, and Denmark added another 18, and a variety of other countries contributed the remaining 27 surveys.
Over the next two days, I’ll focus on the US data, then look at the results from the rest of the world.
Again, thanks for contributing!