The continuing rise in geriatric trauma cases seen at trauma centers has necessitated the creation of new infrastructure for evaluating, treating, and assessing outcomes in injured elders. The ability to predict the likely outcome after trauma is extremely important in shaping the management of these patients after discussion with them and their families. Unfortunately, the tools we have for those prognostications are rather complicated, yet rudimentary.
The gold standard to date is TRISS, which combines physiologic data (revised Trauma Score) at the time of first encounter with anatomic injury information (Injury Severity Score). This allows the calculation of a validated probability of survival (Ps).
However, TRISS is unwieldy and frequently cannot be calculated due to missing data. A consortium was created to address these shortcomings. Of course, they chose a name with an unwieldy acronym: Prognostic Assessment of Life and LImitations After Trauma in the Elderly (PALLIATE).
This group developed the Geriatric Trauma Outcome Score (GTOS) in 2015. They recently published a study comparing GTOS with the gold standard TRISS. This could be important since GTOS is easier to calculate, with less opportunity for missing data since it relies only on age, ISS, and presence of blood transfusion.
They calculated outcomes of nearly 11,000 patients at three centers, and found that GTOS worked as well as TRISS. The major advantage was that GTOS requires only three variables:
GTOS = Age + (ISS x 2.5) + (22 if blood transfused in first 24 hours)
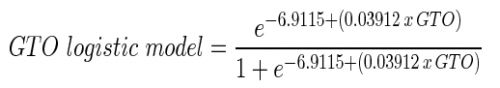
Then, just to make your head spin a little more, the GTO score value gets plugged into this logistic model equation:
Bottom line: GTOS is helpful in some ways, but not in others. It does allow calculation of the probability of survival in elderly patients as well as traditional methods, but with more readily available data points.
However, it is just a probability. It may predict that someone like your patient has a 3% probability of survival, but it cannot tell specifically that your patient is in the 3% vs the 97%. The consortium was trying to make it easier and more objective for clinicians to discuss care plans with family. But this is not really the case.
And a bigger problem is that it gives us no guidance as to quality of life or level of independence for those patients who will probably survive. These factors are, by far, the most important ones when having those hard discussion with patient and/or family. We still need a tool that will guide us on functional outcomes, not just life or death.
Related posts:
Reference: A comparison of prognosis calculators for geriatric trauma: A P.A.L.LI.A.T.E. consortium study. J Trauma, publish ahead of print DOI: 10.109, 2017.

