When trauma patients are enroute to the hospital, accurate arrival times are crucial. If the patient arrives later than announced, the trauma team waits and wastes time. If the patient gets there early, it’s really a form of undertriage and they may not be able to immediately get the critical services they need. A Portland study noted that more than half of transport time estimates were off by at least 10 minutes, and over a quarter were wrong by 10 minutes or more! Surely there must be a way to predict transport time more accurately!
Harbor-UCLA Medical Center developed a simulation using transport data from a single Oregon county for an entire year. Their goal was to determine the factors that influenced transport time and develop a Google Maps application that would be more accurate than current estimates. Route mapping software was used, with inclusion of variables such as patient demographics, use of lights and siren, time of day, and weather. Individual variables that were statistically found to be insignificant were removed, one at a time, until the best model was derived.
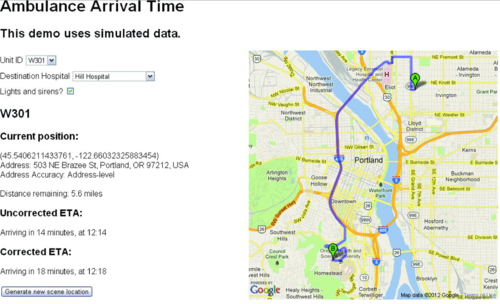
Nearly 50,000 transports were analyzed to create the Google Maps application. Here’s what it looks like:
And here are the interesting findings:
- Without a model, baseline accuracy was only 16% within 5 minutes of predicted
- Transport times were longer during daytime and rush hour (gee!)
- Shorter times occurred with use of lights and siren (gee whiz!)
- Age, sex, wet roads, and trauma system entry had no effect on times
- Use of the model within the Google Maps app increased accuracy to 73% within 5 minutes. Use of lights and siren boosted the accuracy to 78%
Bottom line: Yes, it is possible to enhance the accuracy of arrival predictions of your ambulances. This method should be adopted everywhere! Not only can it improve trauma team use and trauma patient treatment, it can improve ED resource usage for any incoming patient.
Rreference: Predicting Ambulance Time of Arrival to the Emergency Department Using Global Positioning System and Google Maps. Prehospital Emergency Care online first, doi:10.3109/ 10903127.2013.811562.
