Although not strictly traumatic, rectus sheath hematomas frequently come to the attention of trauma professionals. In some cases, they may be due to vigorous physical activity or blunt impact. They may also occur spontaneously, especially in patients who are anticoagulated.
This is not a very common condition, accounting for only 1-2% of patients who present with acute abdominal pain. The common etiology of rectus hematomas is either a tear of the major blood supply (superior and inferior epigastric arteries) or a tear of the muscle itself with bleeding from smaller vessels. The loose attachment of the inferior epigastric and the fixed perforating muscular branches make injury in the lower half of the muscle more common.
These hematomas are frequently self-limiting problems. The rectus sheath provides containment for the hematoma, and as pressure rises, bleeding slows and stops. However, if the hematoma is able to escape posteriorly, it can result in life-threatening bleeding.
Presentation generally consists of abrupt onset of focal abdominal pain, and an abdominal wall mass. The pain can be rather intense, making it difficult to determine if it is intraperitoneal or in the body wall. Tip: ask the patient to tense their abdominal wall muscles, then palpate the area. If the tenderness increases, then it is more likely due to an abdominal wall source. Tensing the muscles will shield sources inside the peritoneal cavity, decreasing tenderness to palpation.
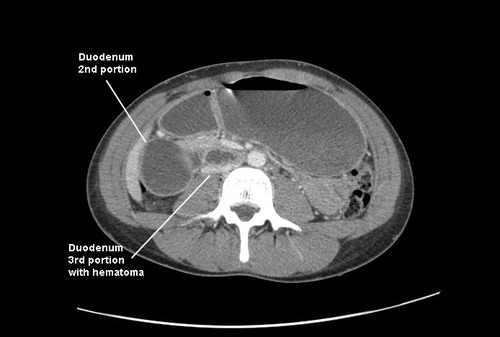
Diagnosis may be made by physical exam, but not always. The hematoma may be seen using ultrasound, but the gold standard is the contrast-enhanced CT. Contrast is essential to determine if active extravasation is occurring.
Ultrasound

CT scan with contrast showing extravasation
Patients who are hemodynamically stable and do not have active extravasation may be treated conservatively. However, a significant number of patients will require at least one unit of blood. Be prepared and send a type and crossmatch. Conservative management includes ice packs for pain relief, direct pressure (sand bags), and reversal of anticoagulation if possible. Stable patients with extravasation on CT should be evaluated by angiography and embolized if a bleeding vessel can be identified.
Unstable patients must be resuscitated promptly with fluid and blood so they can be taken to the angiography suite. Operative exploration is extremely unsatisfying and should be avoided, since it is difficult to find the bleeding vessels in the midst of a huge hematoma.