The management of CSF leaks after trauma remains somewhat controversial. The literature is sparse, and generally consists of observational studies. However, some general guidelines are supported by large numbers of retrospectively reviewed patients.
- Ensure that the patient actually has a CSF leak. In most patients, this is obvious because they have clear fluid leaking from ear or nose that was not present preinjury. Here are the options when the diagnosis is less obvious (i.e. serosanguinous drainage):
- High resolution images of the temporal bones and skull base. If an obvious breach is noted, especially if fluid is seen in the adjacent sinuses, then a CSF leak is extremely likely.
- Glucose testing. CSF glucose is low compared to serum glucose.
- Beta 2 transferrin assay. This marker is very specific to CSF. However, the test is expensive and results may take several days to a few weeks to receive. Most leaks will have closed before the results are available, making this a poor test.
- Place the patient at bed rest with the head elevated. The basic concept is to decrease intracranial pressure, which in turn should decrease the rate of leakage. This same technique is used for management of mild ICP increases after head injury.
- Consider prophylactic antibiotics carefully. The clinician must balance the likelihood of meningitis with the possibility of selecting resistant bacteria. If the likelihood of contamination is low and the patient is immunocompetent, antibiotics may not be needed.
- Ear drops are probably not necessary. They may confuse the picture when gauging resolution of the CSF leak.
- Wait. Most tramatic leaks will close spontaneously within 7-10 days. If it does not, a neurosurgeon or ENT surgeon should be consulted to consider surgical closure.
References:
- Brodie HA, Thompson TC. Management of complications from 820 temporal bone fractures. Am J Otol, 1997;18:188-197.
- Brodie HA. Prophylactic antibiotics for posttraumatic cerebrospinal fluid fistulas. Arch Otolaryngol Head, Neck Surg. 123:749-752.
The management of CSF leaks after trauma remains somewhat controversial. The literature is sparse, and generally consists of observational studies. However, some general guidelines are supported by large numbers of retrospectively reviewed patients.
- Ensure that the patient actually has a CSF leak. In most patients, this is obvious because they have clear fluid leaking from ear or nose that was not present preinjury. Here are the options when the diagnosis is less obvious (i.e. serosanguinous drainage):
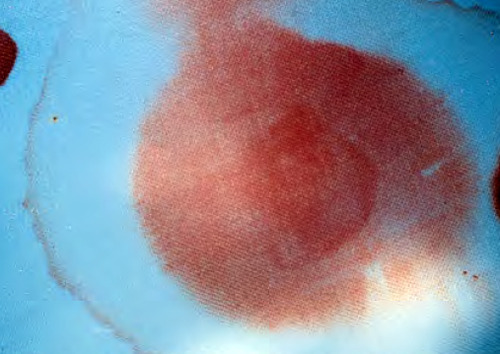
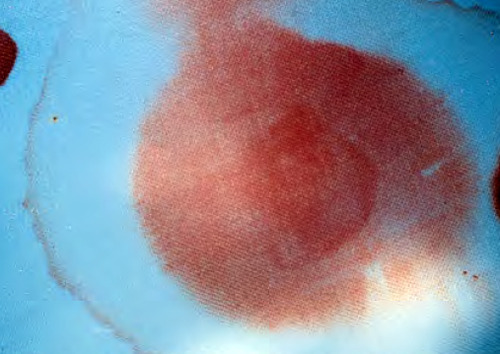
- The “halo” or “double ring sign" is a form of pillow chromatography. The blood components separate from the CSF as they move through the pillow fabric, creating a clear ring or halo surrounding a bloody spot. This is the cheapest, fastest test and is actually fairly reliable.
- High resolution images of the temporal bones and skull base. If an obvious breach is noted, especially if fluid is seen in the adjacent sinuses, then a CSF leak is extremely likely. This test does not usually change management.
- Glucose testing. CSF glucose is low compared to serum glucose. Cheap but hard to obtain a decent specimen.
- Beta 2 transferrin assay. This marker is very specific to CSF. However, the test is expensive and results may take several days to a few weeks. Pricey, and most leaks will have closed before the results are available, making this a poor test.
- Place the patient at bed rest with the head elevated. The basic concept is to decrease intracranial pressure, which in turn should decrease the rate of leakage. This same technique is used for management of mild ICP increases after head injury.
- Consider prophylactic antibiotics carefully. The clinician must balance the likelihood of meningitis with the possibility of selecting resistant bacteria. If the likelihood of contamination is low and the patient is immunocompetent, antibiotics may not be needed.
- Ear drops are probably not necessary. They may confuse the picture when gauging resolution of the CSF leak.
- Wait. Most tramatic leaks will close spontaneously within 7-10 days. If it does not, a neurosurgeon or ENT surgeon should be consulted to consider surgical closure.
References:
- Brodie HA, Thompson TC. Management of complications from 820 temporal bone fractures. Am J Otol, 1997;18:188-197.
- Brodie HA. Prophylactic antibiotics for posttraumatic cerebrospinal fluid fistulas. Arch Otolaryngol Head, Neck Surg. 123:749-752.
The management of CSF leaks after trauma remains somewhat controversial. The literature is sparse, and generally consists of observational studies. However, some general guidelines are supported by large numbers of retrospectively reviewed patients.
- Ensure that the patient actually has a CSF leak. In most patients, this is obvious because they have clear fluid leaking from ear or nose that was not present preinjury. Here are the options when the diagnosis is less obvious (i.e. serosanguinous drainage):
- High resolution images of the temporal bones and skull base. If an obvious breach is noted, especially if fluid is seen in the adjacent sinuses, then a CSF leak is extremely likely.
- Glucose testing. CSF glucose is low compared to serum glucose.
- Beta 2 transferrin assay. This marker is very specific to CSF. However, the test is expensive and results may take several days to a few weeks to receive. Most leaks will have closed before the results are available, making this a poor test.
- Place the patient at bed rest with the head elevated. The basic concept is to decrease intracranial pressure, which in turn should decrease the rate of leakage. This same technique is used for management of mild ICP increases after head injury.
- Consider prophylactic antibiotics carefully. The clinician must balance the likelihood of meningitis with the possibility of selecting resistant bacteria. If the likelihood of contamination is low and the patient is immunocompetent, antibiotics may not be needed.
- Ear drops are probably not necessary. They may confuse the picture when gauging resolution of the CSF leak.
- Wait. Most tramatic leaks will close spontaneously within 7-10 days. If it does not, a neurosurgeon or ENT surgeon should be consulted to consider surgical closure.
References:
- Brodie HA, Thompson TC. Management of complications from 820 temporal bone fractures. Am J Otol, 1997;18:188-197.
- Brodie HA. Prophylactic antibiotics for posttraumatic cerebrospinal fluid fistulas. Arch Otolaryngol Head, Neck Surg. 123:749-752.
Home of the Trauma Professional's Blog